News Category: Outbreak response

In 2003, Melissa Corkum received a call that would change her life. The World Health Organization wanted to interview her for a position in their polio eradication team. Like most people who are hearing about polio eradication for the first time, the story compelled her, and she packed her bags to embark on a new adventure. Seventeen years later, she remains a dedicated champion of polio eradication.
A self-proclaimed ‘virus chaser’, Melissa has worked in all three polio endemic countries – Afghanistan, Pakistan and Nigeria. She found inspiration in her first field job in Nigeria, where she realized the scale of the polio eradication programme and that she was a part of something tremendous in public health history.
“I was amazed and inspired when I first saw the efforts of the front-line workers delivering vaccines to the doorstep. It may seem simple to deliver a couple drops into a child’s mouth, but when you see it in motion for the first time, it is truly remarkable,” Melissa said.

To this day, Melissa remains in awe of the work required to make ‘reaching every child’ possible. From mobilizing financial resources, to getting vaccines where they need to be while keeping them cool. From the microplanning to ensure all children and their houses are on a map, to the mobilization of champions in support of polio and immunization. Along the way, the stewards of these processes play an essential role to deliver the polio vaccine.
Melissa has worn many hats during her time in polio eradication, but her current role may be the most challenging yet. As the Polio Outbreak Response Senior Manager with UNICEF, she must answer the formidable challenge of containing outbreaks, using her expertise to inform global policy, strategy and operations.
To do this Melissa spent 80% of her time in the field prior to the outbreak of COVID-19, working with partners of the Global Polio Eradication Initiative (GPEI), Ministries of Health and local health workers.
Her work is a mix of challenge and excitement – the challenges of containing outbreaks, including those affected by the COVID-19 emergency – and excitement in developing new tools and methods to overcome the evolving challenges that present barriers to eradicating polio.
“There is never a dull day no matter what hat you may be wearing within this programme. If we are going to put an end to polio for good, we are going to have to fight the fight on a number of fronts – endemics and now the emerging issue of outbreaks in a post-COVID world,” said Melissa.
“The key is a willingness to do whatever it takes to get the job done.”
At times, Melissa felt the weight of the enormous challenges to eradicate polio, especially during her time in Afghanistan, where protracted conflict has complicated efforts to deliver basic services to the most vulnerable. Melissa often reflects on her time as Polio Team Lead there and the emotional rollercoaster she faced trying to stay ahead of the virus, while watching the tragedy of war unfold in the country.
“But when I felt down, I would pick myself up and get ready to face the next challenge. I found hope and inspiration in the resilience of the Afghan people, especially the women who worked in the polio programme, risking their lives and demonstrating a courage that stood out amidst all the difficulties.”

Melissa sees gender as one of the keys to polio eradication. She firmly believes that the only way to tighten the gaps in the system is by involving and empowering women equally in all roles across the programme, and that the only way to reach every child is to ensure their caregivers are equally informed and engaged in the decision making process.
“Unless we involve more women in the programme in certain corners of the world, we will continue to reach the same children and miss the same children, making polio eradication ever more difficult,” Melissa said.
“Change won’t happen if we don’t change the way we think about involving women. We need to listen to their views and open the doors for more women to join and participate equally from the community level and all the way to the leadership, decision-making level.”
Melissa was born in a small town in Nova Scotia, Canada. Her views on the critical involvement of women and gender equality in the polio programme very much align with her government’s Feminist Aid Policy. The Government of Canada has been a long-time champion of polio eradication and recently generously pledged C$ 190 million to assist the GPEI achieve its objectives of polio eradication.
Greater gender equity is one of the legacies that the polio programme is working to leave behind after eradication. Reflecting on her career, Melissa explains what keeps her working to defeat polio after all these years.
“It is so inspiring to be part of something tangible and something that is completely possible if we commit ourselves to doing everything possible to find every last child”.
Related news

“The road to the mountain village was rough. It’s only 50 kilometres, but it took more than 3 hours,” says Dr Fatima Ismail, a disease surveillance officer working in Somaliland. “We were bouncing in the car.”
In early 2020, Dr Fatima’s team headed to a remote village near Djibouti to check on a small boy. The boy’s right arm and leg showed a kind of paralysis that sometimes indicates polio. “The village polio volunteer in this mountainous area, geographically inaccessible, found an acute flaccid paralysis (AFP) case,” Dr Fatima remembers.
When children show signs of this paralysis, it is critical to get stool samples to a laboratory to determine whether they have polio. Polio teams ride camels in the desert or donkeys in the mountains when they have to. They brave conflict to get samples to laboratories. In brutally hot climates, they plug mini-freezers into car dashboards to keep samples cool.
All over the world, polio surveillance systems that have been built up over decades track infection sources, evaluate symptoms and transport samples to the laboratory — despite distance, natural disasters, and sometimes war. Now, disease surveillance network — reaching into the most far-flung corners of the globe — is being tapped to address the COVID-19 pandemic.
“In Somalia, the polio programme pivoted its workforce of thousands of frontline staff to support the effort as the cases of COVID-19 spread. Rapid response teams — made up of disease surveillance officers, community health care workers and volunteers — were trained to educate people about the virus and to test suspected cases. By April 2020, the teams were deployed in the field,” said Dr Mamunur Malik, WHO Representative in Somalia.
“In Somalia’s remote villages, they know us as their polio teams, and once they see us, what comes to their minds is that we’re giving them information about polio,” says Mohamed*, a surveillance officer. “So we also give them information about COVID-19. Social mobilisers tell them about COVID-19 symptoms, how to prevent getting infected, physical distancing, cleaning their hands very well with running water and soap.”
The careful procedures that the teams learned for polio surveillance have been adapted for COVID-19, where the required sample is a naso-pharyngeal swab. “We’ve trained our surveillance people on the case definition and how to collect the samples correctly, from people that meet the definition of a suspected case of COVID-19,” says Dr Fatima. “It’s the same infrastructure. After, when we collect the samples from the patient, we send it to the laboratory in Hargeisa.” WHO has given the laboratory equipment and supplies to test samples for COVID-19.
“As with polio samples, the samples of COVID-19 have to be refrigerated, the ice packs should be VERY cold,” says Mohamed. Teams are used to monitoring the packs’ temperature, even in Somalia’s hot weather.
“The logistical challenges we face with AFP/polio surveillance are still the same. This is the rainy season and the roads tend to be terrible,” says Mohamed. “You can’t get to certain places you normally get to, because of the situation on the road. Most of our vehicles can’t make it through the mud.” In those situations, teams work with other United Nations agencies to arrange special humanitarian flights to ship samples.
Frontline staff put their own lives on the line. In April 2020, the polio team lost a colleague due to COVID-19-related infection. Ibrahim Elmi Mohamed, who joined WHO in 2001, was working as a district polio officer in Lower Shabelle. His tragic death, one of many frontline staff around the world due to COVID-19, reminds us of the risks they face every day they go to work.
“Despite overwhelming challenges, teams are committed to continuing their polio work in tandem with the COVID-19 response. It is critical that polio surveillance continues during the pandemic, as Somalia is also fighting outbreaks of vaccine-derived polio type 2 and 3. With polio vaccination campaigns temporarily paused, the teams must be able to track any resulting spread of poliovirus and get ready to respond as soon as it is safe to do so,” says Dr Malik.
“All of us are still doing polio surveillance at the same time as we do surveillance for COVID-19,” says Dr Fatima. “I used to hear from my colleagues that the polio surveillance system is the strongest disease surveillance system. Any polio surveillance team can work in the detection of COVID-19 cases because of the system’s structure, the capacity and experience of the teams.”
Mohamed agrees. “My surveillance coordinator said don’t leave the AFP surveillance behind, follow that normal routine, don’t forget it and leave it aside.’”
As Somalia grapples with the COVID-19 pandemic, its trained teams are working quickly to prevent the spread of both COVID-19 and polioviruses. “What gives me hope in the COVID-19 response is when I look behind and I see what we have done with the polio teams, the impact we’ve had on so many lives,” says Mohamed. “We face everything and we overcome it.”
*Family name withheld for security reasons
Related news

From a small prefabricated container where the walls host detailed maps and desks prop up computer screens beaming data, tables and graphics, the Rapid Response Team at the World Health Organization’s (WHO) Regional Office for Africa coordinate polio outbreak response. The team work across the continent, where 12 countries are battling the vaccine-derived strain of the virus.
Dr Ndoutabe Modjirom, a former Chadian university professor-turned WHO medical officer, coordinates the multi-agency team, which was formed in September 2019. It is composed of twenty experts in operations and vaccination management, epidemiology, logistics, and communications. They are drawn from the core partners of the Global Polio Eradication Initiative (GPEI): WHO, the United Nations Children’s Fund (UNICEF), Rotary International, the US Centers for Disease Control and Prevention, the Bill & Melinda Gates Foundation, and Gavi, The Vaccine Alliance.
The team is mobilized whenever a new polio outbreak is confirmed in the African region.
The first 72 hours
“Our work starts once the lab confirms that a sample collected from either the environment or a paralysed child is caused by a poliovirus. Every minute that passes after the lab confirmation means that the poliovirus is circulating and risks infecting more children,” says Dr Modjirom.
Within the first 72 hours, the Rapid Response Team deploys Team A. This team includes the GPEI Coordinator alongside an epidemiologist, an operations officer, a vaccine manager and a communicator for development. The team works closely with the health authorities in the affected country along with the relevant WHO and UNICEF country offices to prepare a risk assessment and outbreak response plan. The emergency response vaccination campaign, called ‘Round Zero’, starts within 14 days.
Team B takes over from Team A after the first eight weeks and continues the outbreak response activities.
According to standard operating procedures for responding to outbreaks, the polio programme must implement three rounds of high-quality vaccination campaigns in response to every outbreak. Parallel to vaccination, countries must intensify disease surveillance activities to detect new cases of acute flaccid paralysis, a clinical symptom of poliomyelitis.
“Priorities are constantly shifting for the Rapid Response Team,” says Dr Christopher Kamugisha, who has been working with WHO since 1998. He has been a member of the Rapid Response Team since its inception and like the rest of the team has been chasing new polio outbreaks across the region.
“In August I was in Somali Region in Ethiopia supporting the outbreak response, conducting the first vaccination campaign round. On the second day of the campaign, Dr Ndoutabe informed me that a new case was detected in Cheporoni in Ghana and asked me to go and provide technical support,” Dr Kamugisha recalls.

Within 24 hours, he was on a plane to Accra through Addis.
“I arrived at noon the next day and went straight to support the national technical team in their preparations and risk assessment. I assisted with ensuring that their plans are in line with the international standard operating procedures set by the GPEI,” Dr Kamugisha says.
No cure for polio
Polio is a viral disease, multiplying in the intestines and transmitted from person to person mainly through a faecal-oral route or, less frequently, through contaminated water or food.
While there is no cure for polio, the disease can be prevented through administration of a simple and effective vaccine. That is why efforts are underway across the country to rapidly boost immunity levels in children and protect them from polio paralysis.
Thanks to the efforts of the GPEI and country governments, no wild poliovirus has been detected anywhere in Africa since 2016. This stands in stark contrast to 1996, a year when wild poliovirus paralysed more than 75,000 children across every country on the continent.
In 2020, the central challenge for the African Region is overcoming outbreaks of circulating vaccine derived poliovirus. Vaccine-derived polioviruses are rare, but can affect unimmunized and under-immunized populations living in areas with inadequate sanitation and low levels of polio immunization.
Countries experiencing outbreaks of vaccine-derived poliovirus in Africa are Angola, Benin, Cameroon, Central African Republic, Chad, Côte d’Ivoire, Democratic Republic of the Congo, Ethiopia, Ghana, Nigeria, Togo and Zambia. Reasons these outbreaks have occurred include weak routine vaccination systems, vaccine hesitancy, difficulty accessing some locations and low-quality vaccination campaigns, which have made immunization of all children challenging.
In addition to the response activities, the Rapid Response Team work to build the capacity of health workers and decision makers in countries that are not experiencing polio outbreaks, training them to be ready to respond if virus is ever detected.
The team also aims to recruit more women with expertise in outbreak response. Achieving gender balance amongst personnel through a more equitable recruitment process forms part of the GPEI Gender Equality Strategy 2019 – 2023, which was launched in May 2019.
By supporting countries during outbreaks, and building health system resilience in vulnerable settings, the polio programme is working to establish a sustainable legacy that will improve health long after global eradication of the virus.
Related resources
In Karachi’s Gadap Town, many families lack basic health and municipal services. To fill the gap, the Polio Emergency Operations Centre in Pakistan’s Sindh province has recently renovated an abandoned hospital to create an Emergency Response Unit (ERU). The unit provides polio vaccination to communities alongside PolioPlus activities to improve overall health. The unit was built with the support of Rotary International, WHO, UNICEF and the Bill & Melinda Gates Foundation.
Click through the gallery to see how the Gadap Emergency Response Unit has changed health delivery:
Compared to the busy streets of Hargeisa, Somaliland, just 20 kilometres outside of the city are broad stretches of barren land—home to the nomads. Nomadism is part of Somalia’s culture, and there are thousands of families throughout the country who lead pastoral lifestyles, raising livestock and moving their animals and families as the seasons change. Their frequent movement means that children are not always nearby a health clinic to receive their scheduled vaccinations on time. Such disruption or delay in receiving vaccines can result in low or no protection against common childhood infections.
If children are not immunized against polio, they risk contracting the virus and developing paralysis. They also risk passing polioviruses to other under-immunized children. But the polio eradication teams are committed to reach every last child with polio vaccine notwithstanding challenging terrains.
Look through the lives of polio vaccinators in Somaliland on the third day of the vaccination campaign activities as part of the larger efforts to reach over 1.1 million children with the oral polio vaccine.
Related resources
Environmental surveillance teams in Mogadishu access the underground closed drainage system to collect sewage waste water samples, which they package and send to the laboratory for testing. If poliovirus is identified in a sample, epidemiologists know that the disease is likely to be circulating amongst the community whose sewage drains into that part of the system. This process is called environmental surveillance and is one of the most important tools for the polio programme to help detect poliovirus.
Vaccinating every child and conducting disease surveillance to know where the poliovirus is circulating are key strategies to end the outbreak. Low immunization coverage has led to an outbreak of vaccine-derived poliovirus in Somalia. This can occur in places where not enough children have received their full vaccine doses.
The teams must follow best practice to collect samples, to ensure that any poliovirus present can be detected.
Click through this photo gallery to learn more about the sample collection process.
Related News

“Our area is a pretty difficult terrain because we live in the water and it is not easy for the teams coming from outside the community to gain access. So, the (hand-drawn) maps make it possible for us to identify areas we have yet to reach during the immunization exercise”, says Peter Idowu, a veteran community mobilizer and team supervisor in Makoko — a riverine shanty town located on the coast of mainland Lagos city, southwest Nigeria. Native to the village, Peter is the man to go to whenever the polio immunization teams face challenges navigating the waterways or the community.

The sprawling water city Makoko is a slum located across the Third Mainland Bridge on the lagoon. It is a largely low-income community with half the population on water and the other half on land. Informal, makeshift houses with corrugated iron roofs sit precariously atop stilts. Down below, narrow wooden boats act as a form of aquatic taxi ferrying goods and people around the bustling community. Nobody knows the exact population of this slum district of Lagos, but it is estimated to be as high as 100 000. It is mostly a fishing community inhabited by the Egun people.
“My goal is to see that all the kids in our community are immunized and live healthy lives. That is why I engage our teams in sensitizing parents all the time on the importance of routine immunization and the dangers of polio. As a member of the community and with a passion of becoming a health worker myself, I kept on mobilizing our people for easy accessibility, because our language is different from Yoruba and most of the Polio teams can’t speak the language. It is always easy with me being in the Polio team as our people will readily accept the vaccine without rejecting,” says Peter.
Nigeria is the only country in Africa and one of the only three in the world endemic to wild poliovirus, alongside Afghanistan and Pakistan. Nigeria is also affected by circulating vaccine-derived poliovirus type 2 (cVDPV2) outbreaks.
UNICEF works closely together with Global Polio Eradication Initiative (GPEI), key polio partners and the Nigerian government. There is a vast network of over 20 000 community mobilizers focusing on demand creation and improving health-seeking behaviors of caregivers.
Related resources
Amidst a poliovirus outbreak in Papua New Guinea, legions of women health workers and leaders are playing a critical role in ensuring children are fully protected from lifelong paralysis. In the current emergency outbreak response, women have emerged as a strong, reliable, and a decisive group that continue to administer key services in the outbreak response implementation. From medical doctors to surveillance officers to community mobilizers to health workers, women are active and present on all fronts.
World Immunization Week—celebrated in the last week of April— aims to encourage the use of vaccines as one of the safest methods to protect against diseases, including poliovirus. This year’s theme – Protected Together: Vaccines Work! – highlights “heroes” who are ensuring that people of all ages, all across the world are protected through vaccines. Women on the frontlines of the outbreak response in Papua New Guinea are a fitting example who continue to inspire the public health community across the world.
Here is a roundup of some of the extraordinary vaccine “heroes”:

Dr Fiona Kupe
Dr Fiona Kupe is a Paediatric Medical Officer at the Gerehu General Hospital in the National Capital District, Papua New Guinea. She is, in effect, a one (wo)man army as she dons multiple hats in the polio eradication efforts in her home country by searching for children with acute-flaccid paralysis (AFP) at Port Moresby General Hospital and Gerehu General Hospital. She also leads the mapping of communities – or microplanning – for all Supplementary Immunization Activities (SIAs) across three districts.
Along with that, she finds time to train vaccinators and community volunteers, all the while carrying out her clinical duties as a child specialist.
“As a paediatric doctor and a mother…every day, I keep (my) passion alive to overcome challenges and basically to do everything I can to check on children’s vaccination status whenever they come to see me for check-up. As a mother, I know that vaccines save lives. I want my child to survive with good health and I would definitely want the same for all the mothers and children I see.”
Melanie Serei
Seen most days with her trusty pet dog by her side, Melanie works in one of the most challenging areas for immunization activities as a health worker in a remote village of Terapo in Kerema, Gulf province. Geographical inaccessibility aside, Melanie constantly juggles issues of insecurity, violence and community vaccine hesitancy. But, she tries every single day to overcome barriers in her mission to reach every last child with the life-saving polio vaccination.
Building community trust and demand for vaccination were considered key tenets in the risk communication for the polio outbreak response. Melanie successfully carried out door-to-door checks on all the children in the village. Thanks to her diligence, she was quickly able to notice polio symptoms in a child that allowed adequate and rapid actions.
Dr Winnie Sadua
Working as a paediatrician in Angau Memorial General Hospital in Morobe province, Dr Winnie treats one very special patient: six-year-old Gafo—the first reported case of polio in PNG in over 18 years, triggering a national outbreak emergency.

Since his diagnosis, Gafo has gone on to become somewhat of a celebrity, a symbol of hope, and a staunch advocate for polio eradication. Through timely treatment and physiotherapy by Dr Winnie, Gafo can now walk with his signature gait. He is now healthy and excited to start school next year.
With all the patients that come to her, Dr Winnie makes sure to remind all the parents to take heed from Gafo’s case and get their children vaccinated.
Related resources

A new circulating vaccine-derived poliovirus type 2 (cVDPV2) outbreak has been confirmed in Mozambique. Two genetically-linked circulating vaccine-derived poliovirus type 2 (cVDPV2) isolates were detected from an acute flaccid paralysis (AFP) case (with an onset of paralysis on 21 October 2018, in a six-year old girl with no history of vaccination, from Molumbo district, Zambézia province), and a community contact of the case.
As polio is a highly infectious disease which transmits rapidly, there is potential for the outbreak to spread to other children across the country, or even into neighbouring countries, unless swift action is taken. Global Polio Eradication Initiative and partners are working with country counterparts to support the local public health authorities in conducting a field investigation (clinical, epidemiological and immunological) and thorough risk assessment to discuss planning and implementation of immunization and outbreak response.
In January 2017, a single VDPV2 virus had been isolated from a 5-year old boy with AFP, also from Zambézia province. Outbreak response was conducted in the first half of 2017 with monovalent oral polio vaccine type 2 (mOPV2).
Read our Mozambique country page to see information on cases, surveillance and response to the developing outbreak.
Related resources

From the 27 – 29 November, the Technical Advisory Group (TAG) met in Nairobi to review the outbreak response in Somalia, Ethiopia and Kenya, and preparedness measures in Yemen, Uganda, Tanzania, Sudan, South Sudan and Djibouti in case of international spread.
Jean-Marc Olivé, Chairman of the TAG, spoke to WHO about the recommendations made to address the challenges faced by countries, his hopes for eradication and his life in the programme.
What are the main challenges faced by the countries of the Horn of Africa in the drive to stop the outbreaks?
The major challenges have been the same for a long time – like, the issue of inaccessibility due to conflict and humanitarian crises. If we cannot access populations then it is very difficult to cover them properly during vaccination campaigns and so it is hard to stop poliovirus transmission. This is not a programme-related issue, it is a political one. Until we have access, it will be very difficult to make it.
I have said it before and I will say it again: access is success.
I think the second challenge is – and this is one of the reasons why we still have the transmission of circulating vaccine-derived poliovirus in the Horn of Africa – is persistently low vaccination coverage. There are still remote areas, rural areas, heavily populated urban areas where routine immunization has really never been able to offer the same services and coverage as in more accessible areas with fewer challenges.
Since last TAG meeting in the Horn of Africa, what progress have you seen?
I have seen the capacity really building up in the Horn of Africa. The biggest shift is that we now have collected a lot of data about surveillance, about immunization coverage, vaccination campaigns, communications, and also data by the type of population we are reaching and not reaching. What is missing now, and what was the focus of this TAG, is to use this data to monitor progress and orient the programme toward those difficult areas. We have to use the data to tell us a story about what is happening and what to do next.

What were the most important recommendations made by the TAG this time around?
I think the most important is to follow the plan that has been set up for the three outbreak countries to interrupt transmission. Secondly, the countries that have not been yet infected by the virus should have a preparedness plan to ensure that if there are any problems they can move swiftly into action.
The Horn of Africa has seen several outbreaks in the past. What must be done to break the pattern and keep the region polio-free once and for all?
They have identified the problems. They just have to implement the solutions! We need to be sharing and analysing knowledge, information, and building capacity at the local level to ensure that we are on the right track to success.
I say to all the countries, go to the areas where you know you have problems and engage local communities and health authorities. Most of the issues can only be addressed at local levels by local people who understand the situation. Help them to do that, and monitor progress.
This is your thirteenth TAG; what have you learned about the process of international review?
First, you have to work as one team in support of National Teams, all agencies together. There cannot be any agency that claims, “This is us, we are doing that, this is WHO, this is UNICEF…”; this is the Global Polio Eradication Initiative, working together with all committed partners, using the competencies that each of them has. If you don’t address issues comprehensively as one, effective interventions are much more difficult to implement.
How long have you worked on polio eradication? What lessons have you learnt from this experience?
I was involved in the eradication of polio in the Americas. We started in 1985. We did it from A to Z in 9 years. We had very good leadership, commitment from the Government and partners, clear guidelines, very strong monitoring, and solid and reactive support to the field. Then we moved on into measles elimination with the same engagement – and the same results.
Because I have seen it happen, I know it is feasible. I think this is what keeps me so motivated. Polio eradication is a fantastic initiative. If we focus on weak and problematic areas within countries, if Governments and Partners continue to be engaged, we will make it. It’s going to be tough, mainly because of inaccessibility.
Is there anything else you want to add?
The people working in this programme, particularly local people working in the countries are amazing. They are the basis of any future public health intervention. In Pakistan and Afghanistan, woman are more and more playing an important role. This is an incredible advancement and an incredible contribution that was previously thought to be impossible.
But nothing is impossible – you just push, go slowly and constructively you will manage to gain ground over the virus.
Related resources

A health worker administering polio vaccine to a young child.
In the wake of a polio outbreak confirmed on June 26 2018, the Government of Papua New Guinea declared polio a national health emergency. It was imperative that all children under the age of five be vaccinated, even those living in the most inaccessible regions of the country.
As part of the outbreak response, a team from Madang Provincial Health Authority, supported by WHO, travelled for over half a day by road and helicopter to reach the Hagahai people who live in the highlands of Madang province in Papua New Guinea, which is one of the most geographically isolated places in the world.
Ever wondered what it is like to be on the forefront of the fight against polio? Watch and learn how the team made their way to the remote mountain top to deliver vaccines.
Related resources

I have spent nearly my whole career working on eradication programmes – first smallpox, then polio. Eradication has been a rewarding career for me because I am so curious to know what is happening in the world. Every time I see a disease that we have worked so long to stop returning, I become so unhappy and know I need to work to stop it.
I worked for the smallpox eradication programme back in the 1970s. I was an epidemiologist – this means that my job was to track the disease and plan how we could stop it.
We used to hold vaccination campaigns at night because then we knew everyone would be at home, and we wouldn’t risk missing a single person. As our cars pulled up out of the dark, people would peer out of their houses to see what was happening. Somalis are very curious! As we brought them the vaccine, occasionally someone would make trouble, but mostly people were pleased to see us.
Somalia was the last country where smallpox was found in the whole world. When I knew we had really ended it in 1977, I was so happy. My name was printed there on the certification document – it was something to be proud of. We had freed the world from smallpox!
I remember one of my friends calling me in 1997 to tell me we were going to eradicate another disease, and that we had to look out for something called ‘AFP’. I thought to myself, what is this ‘AFP’? I hadn’t heard of it. They explained to me that it means acute flaccid paralysis – and that it was the symptom of a disease called polio.
Then one day in 1999, I received a call asking if I would come and work for the second eradication programme in my single lifetime. They said, “If you are ready, we will make you a coordinator. We don’t know if there is polio in Somalia or not, but we want you to come and see.” I jumped at the chance.
We started to search, looking for AFP cases, to collect stool samples and then to send them to the laboratory for testing. And soon, we had confirmation that polio was in Somalia. As soon as we found cases, lots of people came from inside and outside Somalia to help.
By 2002, we found the last case of indigenous polio, and thought the game was won. I even joked to my friends saying, what will we do now that polio is eradicated? They said to me, no – we still have polio in Nigeria, Egypt, Pakistan, many other countries – another case will come. We have to be prepared to stop it if it comes.
And true enough, we had an outbreak in 2005, and again in 2013. Each time we stopped it. Last year, we found circulating vaccine-derived poliovirus type 2. Vaccine-derived polio causes paralysis just like wild polio, and we must eradicate it too.
We started to organize ourselves and held two vaccination campaigns. But then we found another virus – circulating vaccine-derived poliovirus type 3. So now, we are responding to two outbreaks that need different vaccines at the same time. If we miss cases and miss getting vaccines to all children, we can’t stop polio. It is hard, but we will end these outbreaks just as we ended wild polio before.
Eradicating polio has been very difficult – more difficult than it was to end smallpox. I suffered – me and my wife were even kidnapped once. But I am always motivated to keep going. My motivation was never my salary – to stay alive, I need to work. I must know what is going on in my country, if my people are safe. From morning until night, my job is to make sure activities can go on peacefully. My family are my true reason for committing my life to eradication. I have seven children, and 30 grandchildren; I never once missed getting any of them vaccinated. Never.
I am sure that we will finish this job. When we eradicate polio, I will be so happy – I will have been involved in the certification of the second human disease ever to be eradicated. I feel so lucky to have spent my life working for these two eradication programmes; I am proud to tell stories to my grandchildren of my life’s work.
Eradicating polio won’t take a miracle. It is a job. It needs a lot of hard work to end an outbreak. There is no other way – the only way is to work hard, to find cases, and to respond. We hope that in the coming months we will make it. I do believe we will make it. Inshallah.
Related resources:
Efforts to end polio across the WHO African Region came under the microscope at a meeting of the Africa Regional Commission for the Certification of poliomyelitis eradication (ARCC) held in Nairobi, Kenya, from 12 – 16 November 2018.
Seven countries (Cameroon, Nigeria, Guinea-Bissau, the Central African Republic, South Sudan Equatorial Guinea and South Africa) made presentations to the ARCC on their efforts to eradicate polio, presenting evidence on their level of confidence that there is no wild polio in their borders, the strength of their surveillance systems, vaccination coverage, containment measures and outbreak preparedness. Kenya, the host country, alongside the Democratic Republic of the Congo and Namibia, presented updated reports on their efforts to maintain their wild poliovirus- free status.

A total of 109 participants including partners of the Global Polio Eradication Initiative, non-governmental organisations and Health Ministries were in attendance to hear the reports.
The ARCC is an independent body appointed in 1998 by the WHO Regional Director for Africa to oversee the certification and containment processes in the region. It is the only body with the power to certify the Africa region free from wild polio. The African Regional Office and the Eastern Mediterranean Regional Office are the two WHO regions globally that remain to be certified free from wild poliovirus.
Professor Rose Leke, Chair of the ARCC, reflected on the importance of this meeting: “The rich, open and in-depth discussions held this week with each of the ten countries will allow these countries to strengthen ongoing efforts to further improve the quality of surveillance and routine immunization including in security compromised and hard to reach areas as well as in special populations such as nomads, refugees and internally displaced persons.”
Recommendations made
The ARCC, made up of 16 health experts, made recommendations to the ten countries. They noted with concern that outbreaks of circulating vaccine-derived poliovirus in the Democratic Republic of Congo, Kenya, Niger, Nigeria and Somalia were symptoms of low population immunity and varied quality vaccination campaigns. These countries were encouraged to conduct a high-quality outbreak response. Neighbouring countries were advised that they should assess the risk of spread or outbreaks within their borders. Low population immunity was identified as a significant concern, given the risk further emergences of vaccine-derived poliovirus strains.
Inaccessibility and insecurity were also flagged as a significant concern, with limits to the number of children who were being reached with polio vaccines and the coverage of surveillance efforts in affected areas. Countries were advised to scale up strategies that have proved in the past to be effective in the face of these challenges and to build relationships with civil society and humanitarian organisations who could provide immunization services.
Recommendations were made across the board to address chronic surveillance gaps, especially related to factors affecting the quality and transportation of stool samples reaching the laboratory for testing. The introduction of innovative technologies was commended, and a call was made for countries to expand their use, especially in inaccessible and hard-to-reach areas. Countries were also encouraged to accelerate their progress towards poliovirus containment.
In addition, all of the presenting countries received specific recommendations to support their efforts towards improving surveillance, immunization and containment in order to achieve a level that would give the ARCC the confidence needed to declare the region to have eradicated polio.
Dr Rudi Eggers, WHO Kenya Country Representative, said: “I commend all the countries on the efforts that have gone into achieving the results presented in their reports. It gives us hope that eradication is achievable in the midst of the unique challenges faced by all countries. We appeal to all the countries to fully implement all ARCC recommendations.”
Polio eradication efforts in Kenya
Dr Jackson Kioko, Director of Medical Services, the Kenyan Ministry of Health, said: “Kenya has worked hard to rid the country of wild poliovirus, and we will continue to do so until Africa and the world are certified polio-free.”
While Nigeria remains the only country in Africa to be endemic for wild poliovirus, responses are underway to stop outbreaks of circulating vaccine-derived poliovirus in the Democratic Republic of the Congo, Kenya, Niger and Somalia.
The circulating vaccine-derived poliovirus in Kenya was found in a sewage sample in Eastleigh, Nairobi, in March 2018, closely related to viruses found in Somalia. The Ministry Health, with the support of WHO, UNICEF and partners, has done several polio vaccination campaigns since then to ensure that every child’s immunity is fully built and no virus can infect them.
Related Resources

A health worker vaccinating a child in Raqqa, Syria.
In June 2017, some of the first circulating vaccine-derived poliovirus type 2 (VDPV2) cases were reported in Deir Ez-Zor governorate, in eastern Syria, confirming an outbreak of polio. Since then, 74 cases were reported, with the most recent case reported on 21 September 2017.
Despite being a high-risk country with large scale population movements, inadequate health infrastructure, and accessibility issues, the outbreak response was successfully carried out. Health workers reached out to children to raise immunity levels, vaccinate children, and stop the outbreak, regardless of the location or socio-political climate.
An official outbreak response assessment was carried out by experts on global health, virology, and epidemiology, which concluded that the outbreak could now be closed.
“(Disease) Surveillance is stronger today than it was 18 months ago, when the initial cases were detected…so, as we celebrate what is a remarkable achievement in stopping this outbreak, amid very challenging circumstances, we must not lose sight of the risks posed by continued circulation of virus in other parts of our Region,” said Chris Maher, Manager for Polio Eradication in the WHO Eastern Mediterranean Region.
Read the full statement here.
What is polio surveillance?
One of the most challenging aspects of polio eradication is timely disease surveillance: knowing where the poliovirus is lurking, so we can roll out targeted immunization activities quickly and effectively. With new tools, eradicators are getting the information they need in real time.
For the past three decades, there have been two approaches to find polio: passive and active surveillance. Passive surveillance involves health workers routinely reporting cases of acute flaccid paralysis (AFP) as they find them in health facilities. Active surveillance takes place where there is a higher level of concern that polio might be present. Experts go to hospitals, clinics and even community healers to search out cases of AFP. This approach, often called active case searching, reduces the risk that cases are missed due to human error – people forgetting to report AFP or health care workers or community healers not knowing that they need to report the case.
However, in active case search the key steps of detecting, reporting and investigating the case might not always be happening consistently in all health facilities. There can be a delay of two months or more between a child being paralyzed, experts finding out and alerting the polio surveillance system. In an outbreak setting, this can be long enough for the virus to infect and paralyze more children, moving from one area to another. There was an obvious need to make the surveillance system even more reliable and time-sensitive to ensure the polio surveillance framework is as robust as ever.
Never missing a beat again
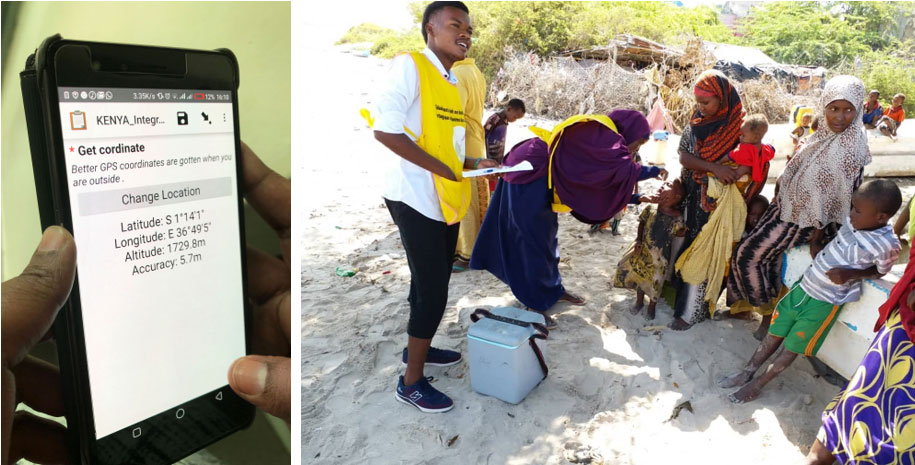
With the Integrated Surveillance and Routine Immunization Supervision system, surveillance officers use an app on their mobile phones to document active case searching as it happens, by tagging the location of every healthcare facility they visit and check.
In order to ensure that active search is conducted timely with real time evidence the polio surveillance systems in Kenya, Ethiopia, Uganda, Eritrea, South Sudan, and Tanzania have adopted an easy-to-use, portable disease surveillance monitoring tool. It delivers unprecedented accuracy across huge areas. The best bit? Most people already have the basic component in their pockets: their mobile phones.
The tool is known as Integrated Surveillance and Routine Immunization Supervision. The idea is simple: surveillance officers use an app on their mobile phones to document active case searching as it happens, by tagging the location of every healthcare facility they visit and check.
“This provides real-time monitoring in the field. Previously, officers would report having done active case searching after the fact – like, ‘I was here and I did x, y, z’. But this is vulnerable to human error in remembering accurately. Sometimes, before we introduced it, someone would go to a distant, rural area and not be able to pinpoint their location on a map for others to follow up. Now, we are sure we are not missing things.” said Christopher Kamugisha, WHO’s Horn of Africa Outbreak Coordinator.
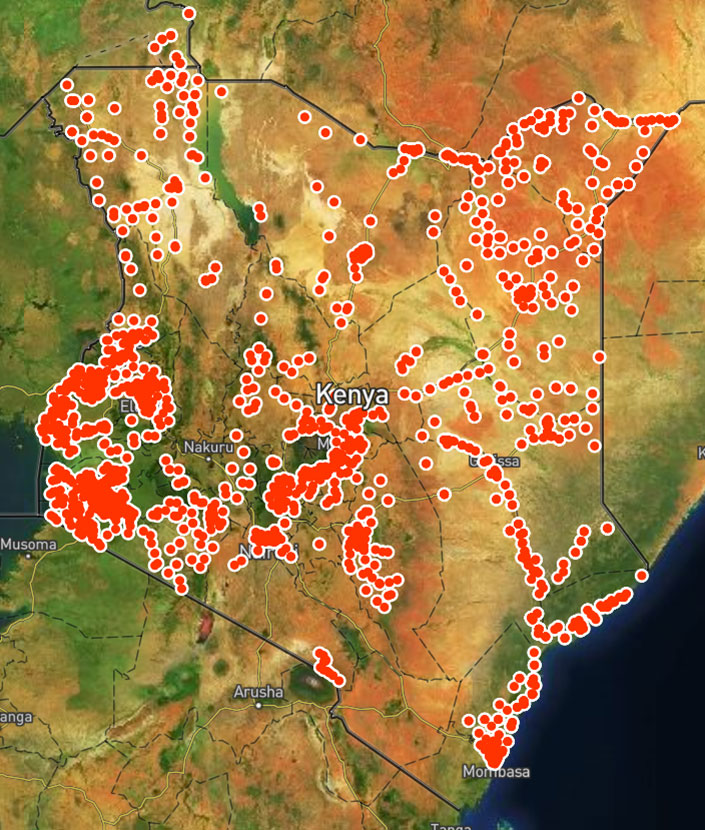
The map that is generated at the national level allows public health experts responding to the polio outbreak the opportunity to see where the gaps in surveillance for polio are in real time.
The app guides surveillance officers through a checklist (questions cover resources available at the facility, polio, measles and routine immunization) that they fill out and send then and there, using their mobile phones, even without an internet connection. It can also provide on-the-spot data analysis so that the surveillance officer can take immediate, evidence-based action.
With a swipe of the screen, users marry surveillance findings to the facility’s location and send the information to a centrally generated map. This gives staff at the national level a clearer picture of where surveillance is working and where it is not, including data on where possible polio cases are, so they know where to direct extra resources.
It also means health workers actively searching for AFP do not have to spend extra time ensuring the information gathered in the field is being shared with the right people for them to take action. For the ongoing outbreak of circulating vaccine-derived poliovirus in the Horn of Africa, this means better disease surveillance – and a better chance to protect children against polio.

For six-year old Gafo that fateful April 2018 morning was supposed to be the start of just another day full of running around and playing with friends. Ignoring the pain in his legs, Gafo tried to get out of bed, but he fell and struggled to get back up. Over the course of the next two days, Gafo’s condition continued to deteriorate. On the third day, Gafo and his family visited the Angau Memorial General Hospital in Lae, Morobe, in the central northern coast of Papua New Guinea, only to find out that he had polio.
As soon as Gafo’s story broke, a National Emergency was declared by the Government and a mass polio vaccination campaign was initiated. Gafo became the foremost champion of polio awareness, and served as a cautionary tale for families and young children to get vaccinated.
Since his diagnosis, Gafo has made progress. Though he can now walk with his signature gait, Gafo and his parents understand that polio is irreversible, but is preventable and eradicable. Gafo hopes to become a doctor one day. Read about his entire journey from being an ordinary child to breaking news, and how his story has helped contain polio in Papua New Guinea.
This story is originally from the Papua New Guinea Polio Outbreak Response First 100 Days report.

To mark the 100 days since the Government of Papua New Guinea launched the Emergency Response to the Polio Outbreak, the National Department of Health, with support from WHO, UNICEF and other partners released a report on the key accomplishments and highlights from of the response operations.
The 100 Days Report is dedicated to the thousands of front line polio workers who braved challenges and worked long hours to ensure that children in Papua New Guinea are protected from polio.
In the Democratic Republic of the Congo, emergency response has been ongoing since 2017 to overcome outbreaks of circulating vaccine-derived poliovirus, caused by low rates of routine immunization. In the battle to close the outbreak, health workers, partners of the Global Polio Eradication Initiative, Governors of affected provinces, and the Ministry of Health are working together to vaccinate every child. In a context with weak health systems and other high-profile health and humanitarian emergencies, these united efforts are crucial to boost population health and keep all young children safe from paralysis.
Reposted with permission from gavi.org.

The first of four large-scale immunization campaigns is set to kick off in Papua New Guinea next week, following last month’s confirmation of a circulating vaccine-derived poliovirus type 1 (cVDPV1). More than 2900 health workers, vaccinators and volunteers have been mobilized to vaccinate almost 300 000 children under 5 years of age in Morobe, Madang and Eastern Highlands provinces. The campaign from 16-29 July is the first in a series of vital immunization campaigns planned every month for the next four months.
“Polio is back in Papua New Guinea and all un-immunized children are at risk,” said Pascoe Kase, Secretary of the National Department of Health (NDOH). “It is critical that every child under five years of age in Morobe, Madang and Eastern Highlands receives the polio vaccine during this and other immunization campaigns, until the country is polio-free again.”
As polio is a highly infectious disease which transmits rapidly, there is potential for the outbreak to spread to other children across the country, or even into neighbouring countries, unless swift action is taken. With no cure for polio, organisers of the immunization drive are calling for the full support of all sectors of society to ensure every child is protected. Parents living in the three provinces are encouraged to bring their children to local health centres or vaccination posts to receive the vaccine, free of charge, during the campaign.
“Everyone has a role to play in stopping this terrible disease,” commented Dr Luo Dapeng, WHO Representative in Papua New Guinea. “We call on parents to bring your children under five years of age for vaccination, irrespective of previous immunization status. Together, we can help ensure that this outbreak is rapidly stopped and that no further children are paralysed by polio.”
The Officer In Charge for UNICEF Representative, Ms. Judith Bruno, stressed, “As long as the polio virus persists anywhere, all un-immunized children remain at risk, and since polio carries enormous social costs, we must make it a key priority to stop its transmission so that children, families and communities are protected against this terrible disease.”
The immunization campaign is organized by the National Department of Health and the Provincial Health Authorities, with support from the World Health Organization (WHO), UNICEF, Rotary International and other partners.
Campaign dates are:
• First Round: 16-29 July 2018
• Second Round: 13-26 August 2018
• Third Round: 10-23 September 2018
• Fourth Round: 8-21 October 2018
Following confirmation of the cVDPV1, on 22 June the National Department of Health of Papua New Guinea immediately declared the outbreak a ‘national public health emergency’, requiring emergency measures to urgently stop it and prevent further children from lifelong polio paralysis. The measures implemented by the government intend to comply fully with the temporary recommendations issued under the International Health Regulations ‘Public Health Emergency of International Concern (PHEIC)’.
Papua New Guinea has not had a case of wild poliovirus since 1996, and the country was certified as polio-free in 2000 along with the rest of the WHO Western Pacific Region. In Morobe Province, polio vaccine coverage is suboptimal, with only 61% of children having received the recommended three doses of polio vaccine. Water, sanitation and hygiene are also challenges in the area, which could contribute to further spread of the virus.