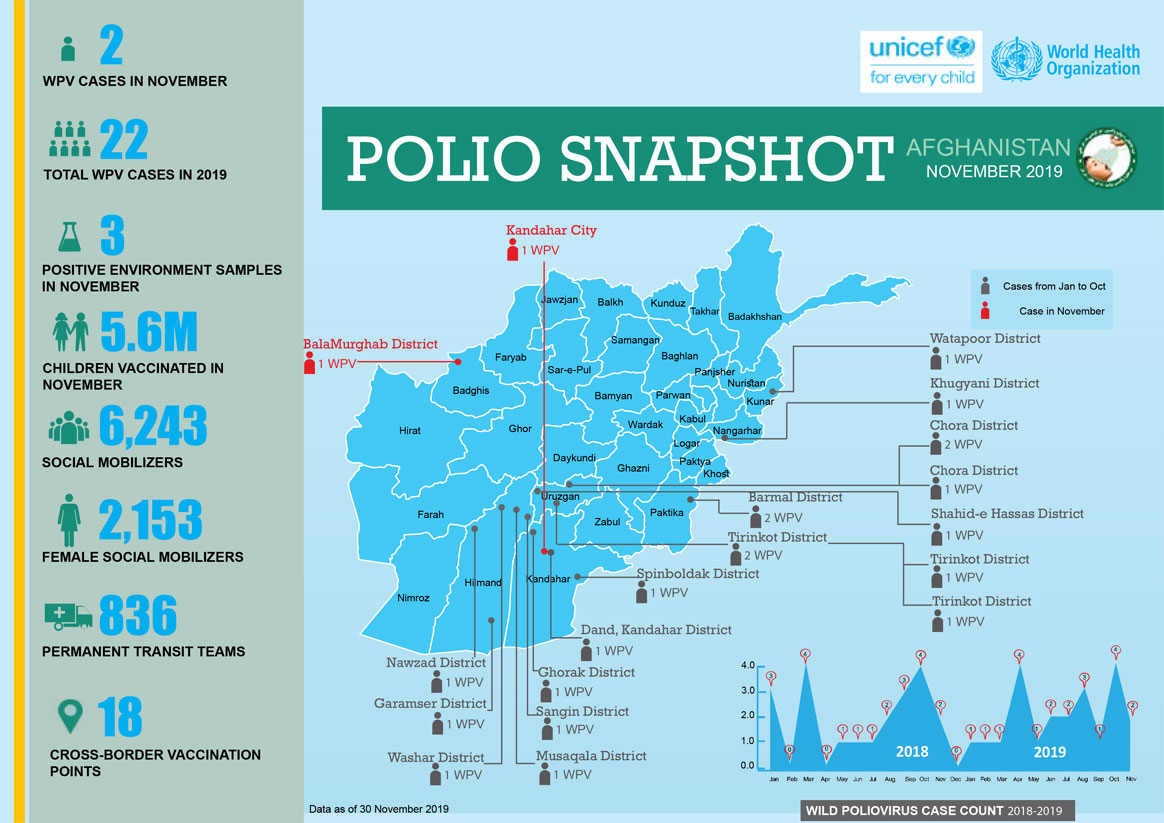
In November:
- Two cases of wild poliovirus were reported
- 5.6 million children were vaccinated.
- Permanent transit teams vaccinated 1,723,859 children and cross-border teams vaccinated 163 775 children
In November:

Q: Outbreaks of circulating Vaccine-Derived Poliovirus type 2 (cVDPV2) are popping up in a lot of countries. How do you explain this? Did the programme know this would happen after the oral polio vaccine ‘switch’?
There have been 47 cVDPV2 outbreaks in 20 countries since the switch in April 2016. Some of these outbreaks are spreading over more than one country. Taking the three years before the switch as a frame of reference, there were 8 cVDPV2 outbreaks in five countries altogether in 2013, 2014 and 2015.
Based on epidemiological modelling studies, we anticipated cVDPV2 outbreaks following the removal of the type 2 component from oral polio vaccine in 2016, via the trivalent to bivalent OPV “switch”. And we anticipated that VDPV cases would outnumber wild poliovirus cases in the endgame. However, what the modelling did not predict was the number and scale of these outbreaks, some of which have proven very difficult to stop.
The reason we are seeing a growing number of cVDPV2 outbreaks, particularly in Africa, is the result of a growing cohort of children without mucosal immunity to type 2 poliovirus, while at the same time the [polio] programme uses monovalent oral polio vaccine type 2 (mOPV2) to respond to existing cVDPV2 outbreaks.
The monovalent vaccine [mOPV2] is currently our only tool to interrupt transmission of cVDPV2 and it is very effective when there is sufficient vaccination coverage in the communities we are targeting to avoid an outbreak. However, when campaign quality is poor and not enough children are reached with the vaccine, we run a risk of seeding new viruses among under-immunized populations. There has been evidence of this happening in and outside of outbreak response zones. We are currently developing a new strategy for stopping cVDPV2 outbreaks, and at the same time preventing new outbreaks.
Q: With a limited global stockpile of mOPV2, is there sufficient vaccine to respond to these and future outbreaks?
No. Current mOPV2 stock is insufficient to cater for the number of outbreaks and the sizes of populations requiring it. The GPEI is working with vaccine manufacturers to boost production of mOPV2 and we expect to meet targeted quantities in 2020.
The vaccine will continue to be used for cVDPV2 outbreak response until a new and more genetically stable oral polio vaccine, known as novel oral polio vaccine type 2 (nOPV2), currently under clinical development, is available.
Q. What does increased production of mOPV2 mean for vaccine manufacturers in terms of containment? On one hand, the polio programme is asking for more live type 2-containing OPV. And on the other, it’s pushing for strict containment of all type 2 wild and Sabin polioviruses.
It’s a balance. The world needs enough mOPV2 stocks to help with the elimination of cVDPV2, and type 2 live attenuated poliovirus is needed to produce this vaccine. Yes, we are asking vaccine manufacturers to make more vaccine, but [vaccine] production and containment of type 2 virus are not mutually exclusive pursuits. Polio vaccine manufacture is costly, particularly when demand calls for rapid scale-up of outputs. Containment is also costly. But this is not a reason to put it on hold and stop efforts to ensure safe and secure handling and storage of virus. Quite the opposite: the impetus for putting in place adequate biorisk management systems should be greater, given the higher level of risk of human exposure to poliovirus in and around these facilities.
Q. What about manufacturers of inactivated polio vaccine (IPV)? Can they afford to relax?
IPV is made with killed, or inactivated strains of wild poliovirus types 1, 2 and 3, or their Sabin counterparts. Any facility manufacturing polio vaccines using the type 2 serotype – be it wild or Sabin ̶ and type 3 wild poliovirus since the declaration of its global eradication in October, is required to implement containment measures set out by WHO. This of course also applies to any other type of facilities holding the viruses, for example, research or diagnostic labs.
Holding on to these viruses is a risk and responsibility, and appropriate measures must be taken to protect communities from reintroduction and resurgence.
The world needs IPV and will continue to need it for the foreseeable future. We need vaccine production to continue in well-managed facilities that incorporate GAPIII approaches to biorisk management.
Q. of Sabin 2 remains a priority, while simultaneously, mOPV2 made up of Sabin 2 is being used in countries around the world. What gives?
First, we must be clear that use of mOPV2 is not a decision that is taken lightly. A thorough risk-benefit analysis is conducted before an advisory committee makes a recommendation and it is submitted to the Director-General of WHO for his approval.
It is never ideal to use mOPV2 and reintroduce Sabin 2, which should be under containment. However, as I mentioned earlier, mOPV2 is currently the only tool available to stop outbreaks of cVDPV2 and we must use it.
The reason we continue to push for containment of Sabin 2 viruses in countries not experiencing cVDPV2 outbreaks is precisely to prevent further emergences of VDPV2, which can cause outbreaks of cVDPV2 more easily now because of the very low population mucosal immunity to type 2 poliovirus.
Q. sounds like we are fighting fire with fire with mOPV2. Are we?
Many outbreaks have been stopped using mOPV2. However, in areas with low routine vaccination coverage, and thus low immunity, we are indeed reintroducing Sabin 2 in naïve populations and seeding new outbreaks. We are currently reviewing all aspects of our cVDPV2 approach and developing a new strategy that examines all options and tools ensuring we are using each for full impact. This includes improving our outbreak response so that it is appropriate in scope and effective, and accelerating the development and roll-out of a new vaccine that is less likely to seed outbreaks.
Q: When will nOPV2 be available?
Clinical trials are underway. There are numerous influencing factors but if all goes according to plan, our estimate is that approximately 100 million doses of the vaccine could be ready by mid-2020, with another 100 million by the end of the year. We are also working with the WHO prequalification team, which independently reviews all vaccine data to ensure a consistent quality in accordance with international standards to enable the vaccine to be used as quickly as possible by affected countries under an Emergency Use Listing (EUL), a risk-based procedure for assessing vaccines for use during public health emergencies—such as polio.
The vaccine is also being developed for types 1 and 3 polioviruses; however, this is further away in terms of production.
Reposted with permission from Rotary.org.

When we talk about PolioPlus, we know we are eradicating polio, but do we realize how many added benefits the programme brings? The ‘plus’ is something else that is provided as a part of the polio eradication campaign. It might be a hand-operated tricycle or access to water. It might be additional medical treatment, bed nets, or soap.
This series looks at the ‘pluses’ that Rotarians worldwide help to provide. Our first article looked at prevention of other diseases, and in part two we investigated how Rotary contributes to clean water provision. In our final article, we consider how Rotarians support those who have contracted polio, and who now live with permanent paralysis.
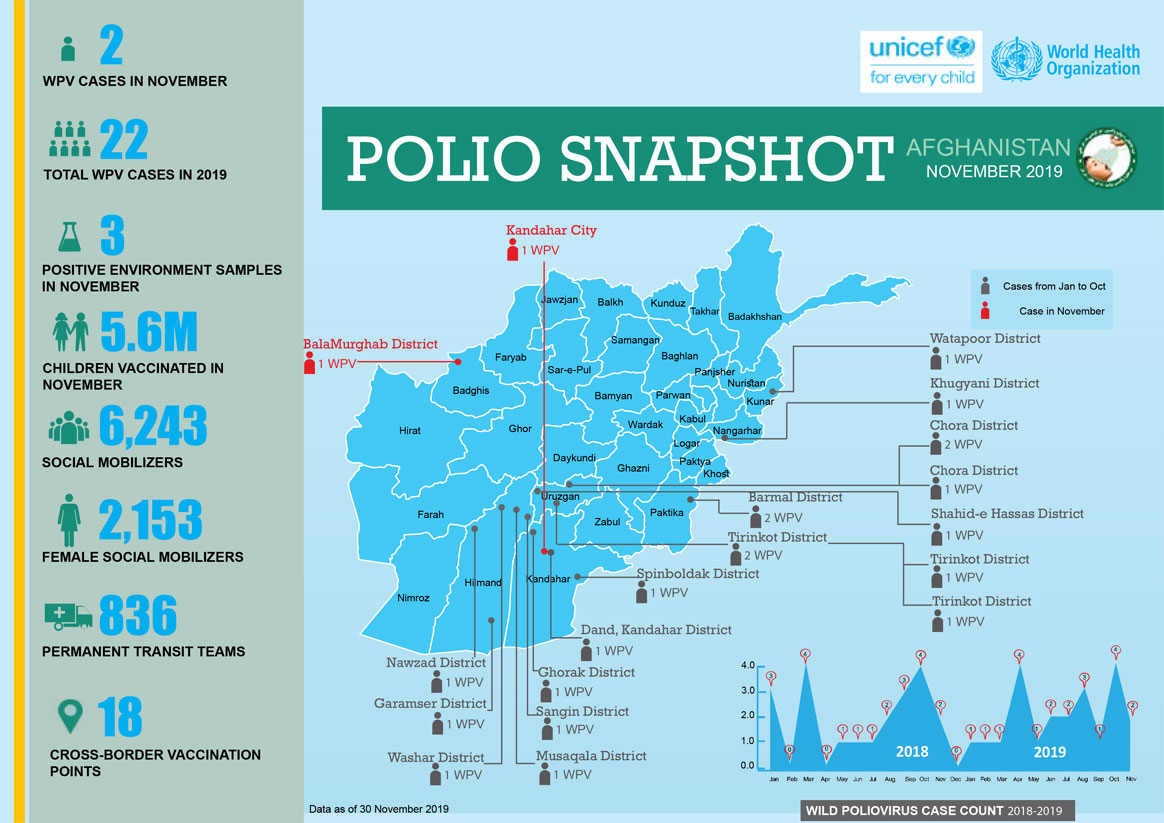
Creating jobs
Polio paralysis left Isiaku Musa Maaji, who lives in Nigeria, with few ways to make a living. At 24, he learned to build hand-operated tricycles designed to provide mobility for adults and children with physical disabilities, and later started his own business assembling them. His first break came, he says, when his local government placed a trial order. Officials were impressed with his product, and the orders continued.
Rotary’s Nigeria PolioPlus Committee recently ordered 150 tricycles from Maaji to distribute to polio survivors and others with mobility problems. The relationship he has built with local Rotarians has motivated him to take part in door-to-door polio vaccination campaigns.
“It is not easy to be physically challenged,” he says. “I go out to educate other people on the importance of polio vaccine because I don’t want any other person to fall victim to polio.”
Aliyu Issah, another polio survivor, feels lucky; he’s able to support himself running a small convenience store. He knows others with polio paralysis who have attended skills training programmes but lacked the money to start a similar business. In the absence of ready employment, some of them were forced to beg on the street.
He notes however that the polio eradication programme provides a job that is uniquely suited to polio survivors: educating others about the effects of the disease.
“Some of my friends who used to be street beggars now run their own small business with money they earn from working on the door-to-door immunization campaign,” Issah says.
Improving health care
In Maiduguri, Nigeria, Falmata Mustapha rides a hand-operated tricycle donated to her by Rotary’s Nigeria PolioPlus Committee. She is joined by several health workers for a door-to-door immunization campaign, bringing polio drops to areas without basic health care.

UNICEF data show that polio survivors like Mustapha have a remarkable success rate persuading reluctant parents to vaccinate their children — on average, survivors convince seven of every ten parents they talk to. In places where misinformation and rumours have left people hesitant to vaccinate, the survivors’ role in the final phase of the eradication effort is critical.
“Since working with the team, I have seen an increase in immunization compliance in the community,” Mustapha says. “I am well-regarded in the community because of my work, and I am happy about this.”
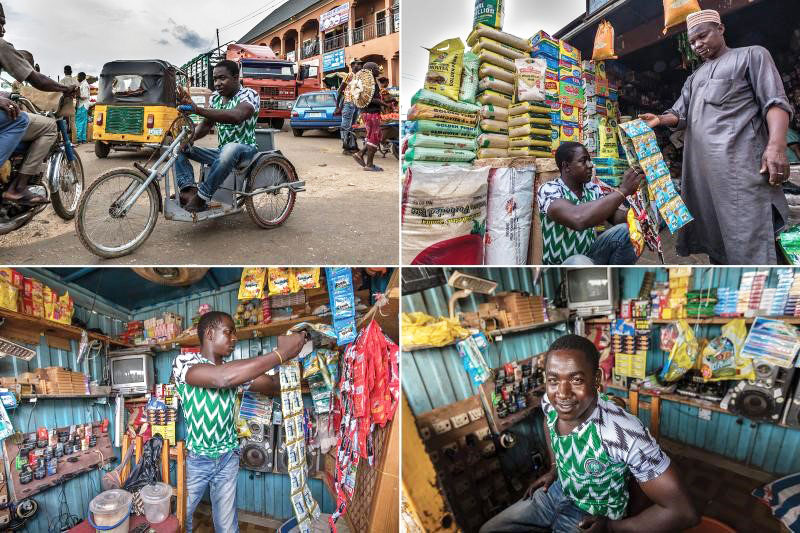
In September
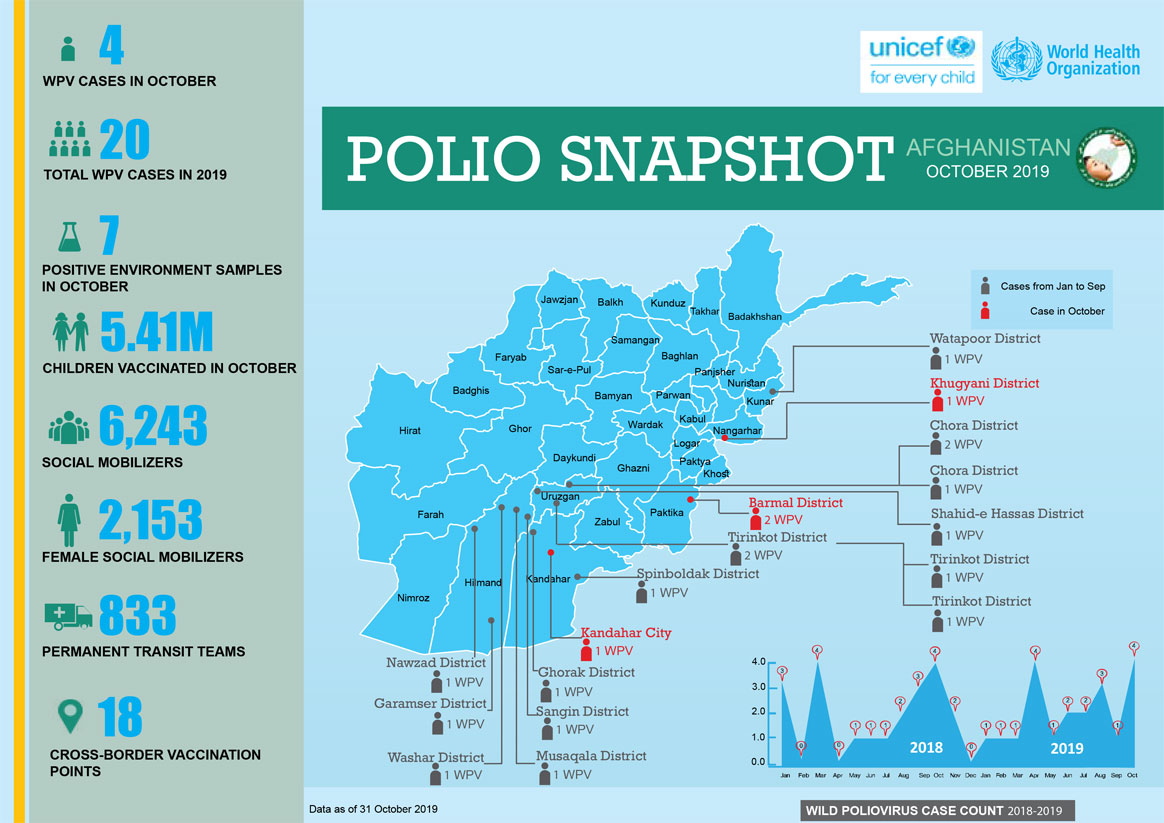
In October:
Reposted with permission from Rotary.org.

When we talk about PolioPlus, we know we are eradicating polio, but do we realize how many added benefits the programme brings? The ‘plus’ is something else that is provided as a part of the polio eradication campaign. It might be a hand-operated tricycle or access to water. It might be additional medical treatment, bed nets, or soap.
This series looks at the ‘pluses’ that Rotarians worldwide help to provide. Our first article looked at prevention of other diseases. In part two, we look at another lifechanging intervention: providing clean water for communities.
Providing clean water
Addressing a critical long-term need such as access to clean water helps build relationships and trust with community members. Within camps for displaced people in northern Nigeria, the polio vaccinators who regularly visit communities are sometimes met with frustration. “People say, ‘We don’t have water, and you’re giving us polio drops,’” Tunji Funsho explains. Rotary and its partners have responded by funding 31 solar-powered boreholes to provide clean water in northern Nigeria, and the effort is ongoing.
Supplying clean water to vulnerable communities is a priority of the PolioPlus programme not only in Nigeria, but also in Afghanistan and Pakistan — the only other remaining polio-endemic nations, where transmission of the virus has never been interrupted.

“Giving water is noble work also,” says Aziz Memon, chair of Rotary’s Pakistan PolioPlus Committee.
Access to safe drinking water is also an important aspect of the The Polio Endgame Strategy 2019-2023, which aims to “ensure populations reached for polio campaigns are also able to access much-needed basic services, such as clean water, sanitation, and nutrition.” The poliovirus spreads through human waste, so making sure people aren’t drinking or bathing in contaminated water is critical to eradicating the disease. Bunmi Lagunju, the PolioPlus project coordinator in Nigeria, says that installing the boreholes has helped prevent the spread of cholera and other diseases in the displaced persons camps.
Communities with a reliable source of clean water have a reduced rate of disease and a better quality of life. “When we came [to the camp], there was no borehole. We had to go to the nearby block factory to get water, and this was difficult because the factory only gave us limited amounts of water,” says Jumai Alhassan, as she gives her child a bucket-bath. “We are thankful for people who provided us with the water.”
By looking holistically at the needs of communities, Rotarians are ending polio, and making a significant contribution to overall health.
This story is part of the Broader Benefits of Polio Programme series on our website, which originally appeared in the October 2019 issue of The Rotarian magazine. Read part one.
The polio eradication campaign needs your help to reach every child. Thanks to the Bill & Melinda Gates Foundation, your contribution will be tripled. To donate, visit endpolio.org/donate.
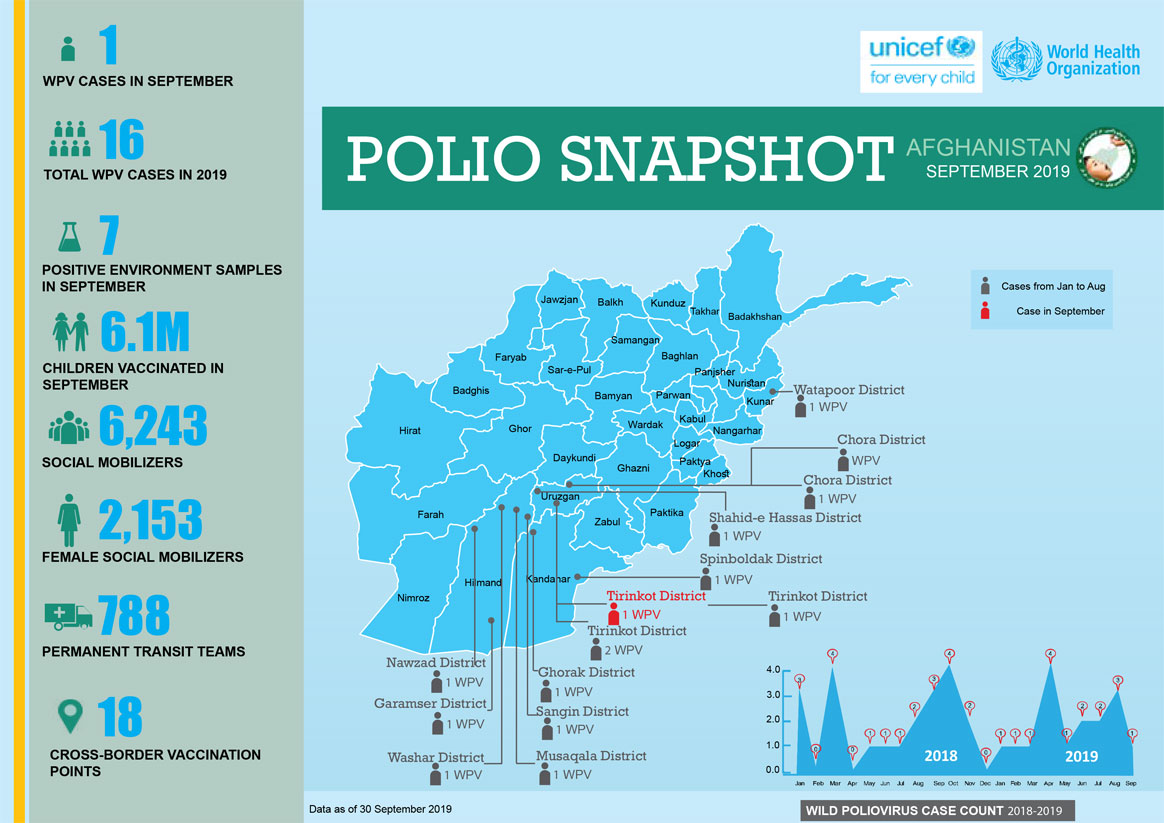
In September:
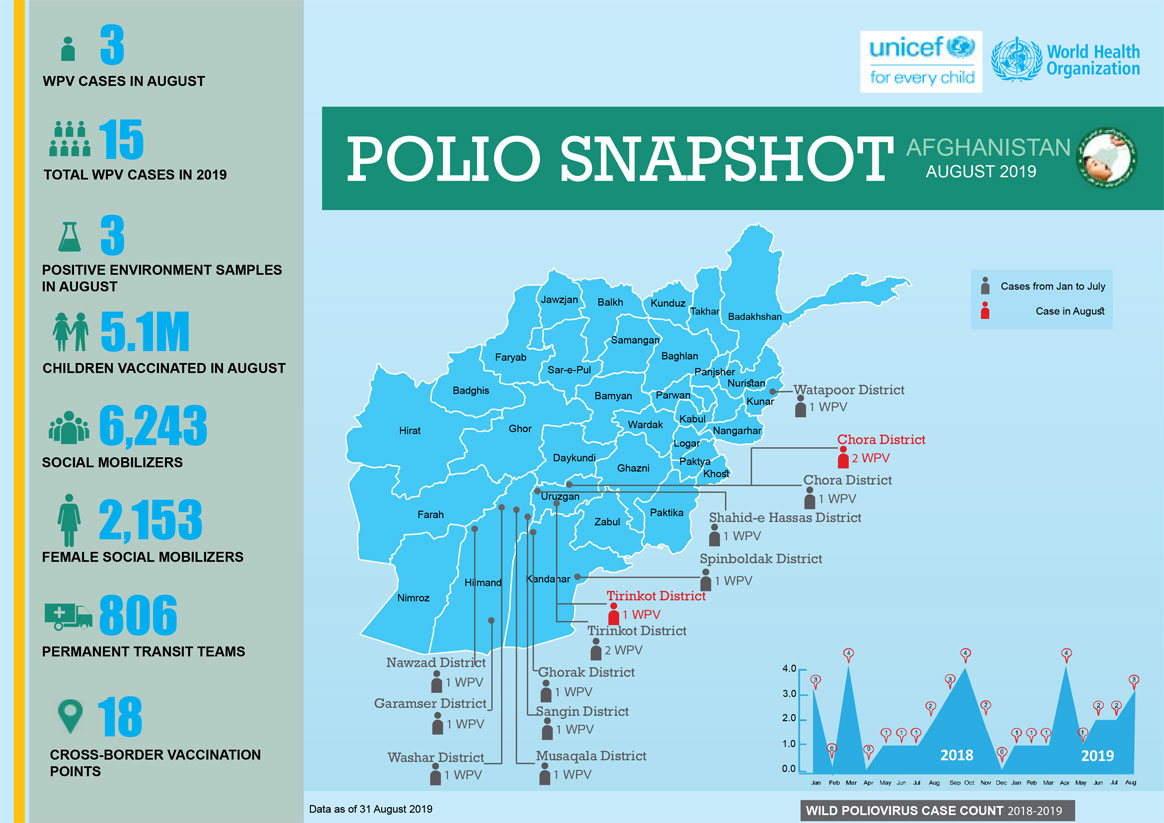
In August:
Reposted with permission from Rotary.org
When we talk about PolioPlus, we know we are eradicating polio, but do we realize how many added benefits the programme brings? The “plus” is something else that is provided as a part of the polio eradication campaign. It might be a hand-operated tricycle or access to water. It might be additional medical treatment, bed nets, or soap. This series takes a look at the ‘Pluses’, starting with prevention of other diseases. A 2010 study estimates that vitamin A drops given to children at the same time as the polio vaccine had at that time already prevented 1.25 million deaths by decreasing susceptibility to infectious diseases.
We take you to Nigeria, which could soon be declared free of wild poliovirus, to show you some of the many ways the polio eradication campaign is improving lives.

Polio vaccination campaigns are difficult to carry out in northern Nigeria, where insurgency has displaced millions of people, leading to malnutrition and spikes in disease. When security allows, health workers diligently work to bring the polio vaccine and other health services to every child, including going tent to tent in camps for displaced people.
The Global Polio Eradication Initiative (GPEI), of which Rotary is a spearheading partner, funds 91% of all immunization staff in the World Health Organization’s Africa region. These staff members are key figures in the fight against polio — and other diseases: 85% give half their time to immunization, surveillance, and outbreak response for other initiatives. For example, health workers in Borno use the polio surveillance system, which detects new cases of polio and determines where and how they originated, to find people with symptoms of yellow fever. During a 2018 yellow fever outbreak, this was one of many strategies that resulted in the vaccination of 8 million people. And during an outbreak of Ebola in Nigeria in 2014, health workers prevented that disease from spreading beyond 19 reported cases by using methods developed for the polio eradication campaign to find anyone who might have come in contact with an infected person.

Children protected from polio still face other illnesses. In Borno, malaria kills more people than all other diseases combined. To prevent its spread, insecticide-treated bed nets — such as the one Hurera Idris is pictured installing in her home above — are often distributed for free during polio immunization events. In 2017, the World Health Organization organized a campaign to deliver antimalarial medicines to children in Borno using polio eradication staff and infrastructure. It was the first time that antimalarial medicines were delivered on a large scale alongside the polio vaccine, and the effort reached 1.2 million children.
Rotary and its partners also distribute soap and organize health camps to treat other conditions. “The pluses vary from one area to another. Depending on the environment and what is seen as a need, we try to bridge the gap,” says Tunji Funsho, chair of Rotary’s Nigeria PolioPlus Committee. “Part of the reason you get rejections when you immunize children is that we’ve been doing this for so long. In our part of the world, people look at things that are free and persistent with suspicion. When they know something else is coming, reluctant families will bring their children out to have them immunized.”
Rotarians’ contributions to PolioPlus help fund planning by technical experts, large-scale communication efforts to make people aware of the benefits of vaccinations, and support for volunteers who go door to door.

Volunteer community mobilizers are a critical part of vaccination campaigns in Nigeria’s hardest-to-reach communities. The volunteers are selected and trained by UNICEF, one of Rotary’s partners in the GPEI, and then deployed in the community or displaced persons camp where they live. They take advantage of the time they spend connecting with community members about polio to talk about other strategies to improve their families’ health.
Nigerian Rotarians have been at the forefront of raising support for Rotary’s polio efforts. For example, Sir Emeka Offor, a member of the Rotary Club of Abuja Ministers Hill, and his foundation collaborated with Rotary and UNICEF to produce an audiobook called Yes to Health, No to Polio that health workers use.
This story is part of the Broader Benefits of Polio Programme series on our website, which originally appeared in the October 2019 issue of The Rotarian magazine.
The polio eradication campaign needs your help to reach every child. Thanks to the Bill & Melinda Gates Foundation, your contribution will be tripled. To donate, visit endpolio.org/donate.
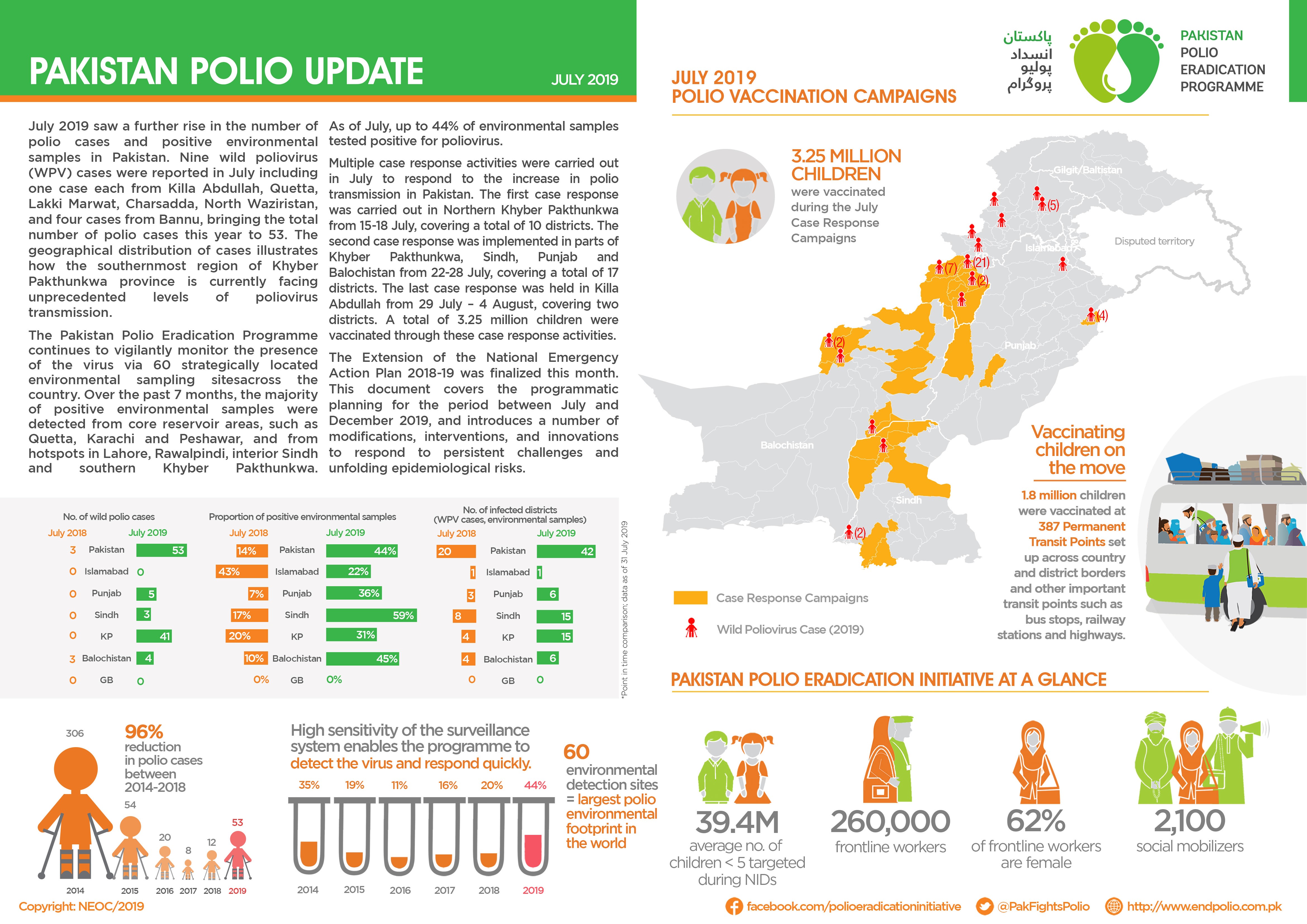
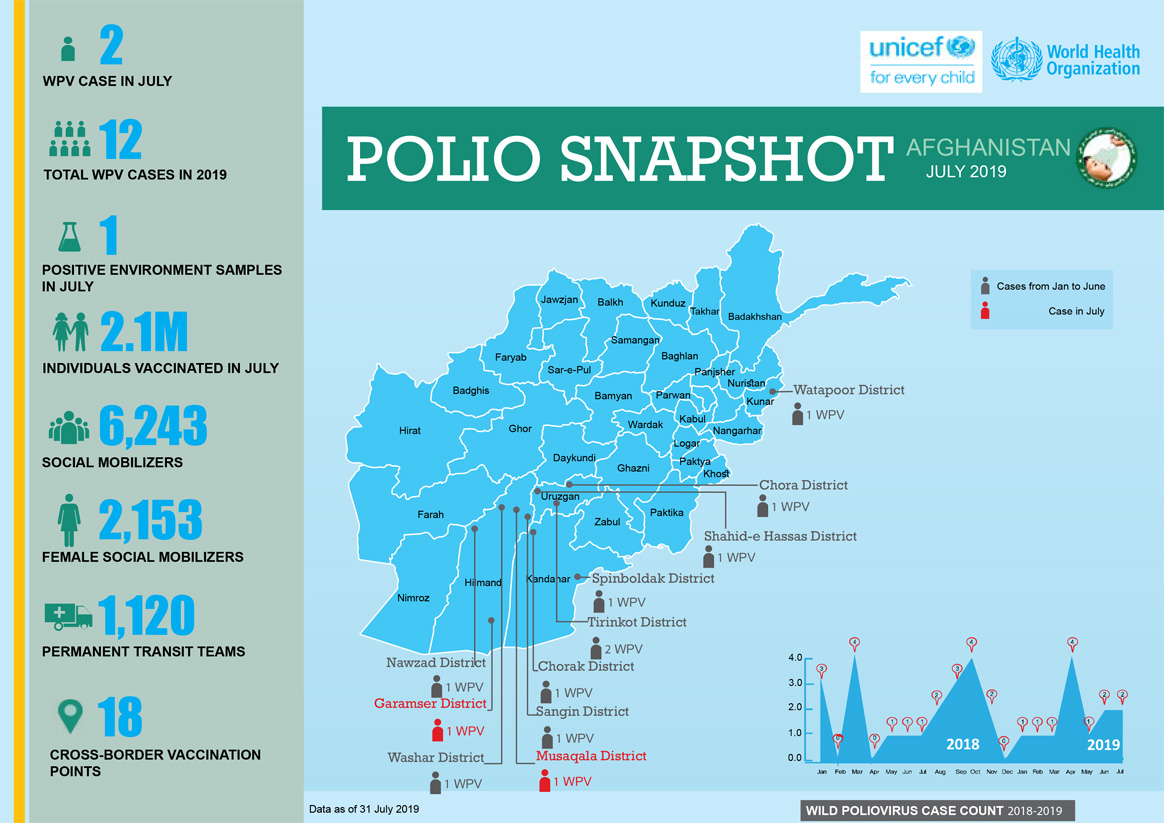
In July

In Union Council Kechi Baig, Quetta district, Balochistan province of Pakistan, Asma needs no introduction. When she talks, people listen. First, when she was one of the few female religious scholars at her local madrassa (school), and of late, as a champion for the polio programme.
For Asma, the segue into community health sensitization was quite natural. Her religious vocation as a teacher, also known as an Alima, and her life-long aspiration to help her community, came full circle when she became a religious support person (RSP) for the polio programme.
“I always wanted to become a doctor… but (it just so happened) I joined a madrassa and became an Alima…when I heard that the polio programme is looking for female RSPs, I took the opportunity. Even though I did not become a doctor, I can workwith doctors to serve humanity,” said Asma about her motivations.
As one of three female RSPs out of a team of 118, she has given unique credence to the polio efforts in her community. Kechi Baig accounts for a significant number of refusals to vaccinate. Community health workers are sometimes unable to make headway with refusal families. In such cases, Asma plays an important role as a faith-based counsellor, drawing upon her knowledge and expertise on religious teachings with communication skills and personal friendships within the community. Asma convinces 15-20 ‘hard refusal’ families in each vaccination campaign.
“I visit the households and leave with grandmothers convinced. As a madrassa teacher, I have seen that most females are unaware of religious teachings of Islam and the role of women to improve society. The polio fatwa (Islamic rulings) book proves to be very helpful because it contains authentic fatwas from venerated religious scholars.”

Re-appropriating polio through a religious lens
Asma realizes that bringing an attitudinal change through one-off encounters with refusal households is not enough. She saw the need for a long-term counselling relationship. Now, the polio programme team also conducts community engagement sessions with a cross-section of women across the community — from mothers to grandmothers to young students to women training at Asma’s madrassa—to raise awareness about polio.
“It is a great achievement being part of the training sessions about polio and health where I get to talk about the fatwa book. In almost every campaign I work with community health workers and convince 15 to 20 hard refusals for vaccination. It’s a big opportunity to save children from polio,” explained Asma.
Religious support persons, particularly women RSPs like Asma, play a very important role in mediating how people consider their choices for and against polio vaccination through the religious interface. By incorporating educative, spiritual, and medical knowledge, faith-based counselling goes a long way in neutralizing any refusal predispositions within the community.

21 August 2019 marks three years since Nigeria last reported a case of wild poliovirus. This is an important public health milestone for the country and the entire Africa Region, which is now a step now closer to polio-free certification.
At the press conference in Abuja, the Executive Director of the National Primary Health Care Development Agency (NPHCDA), Dr Faisal Shuaib, acknowledged that the three-year mark is an important moment in the fight against polio but also emphasized the need for vigilance ̶ “one which we must delicately manage with cautious euphoria.”
“This achievement would certainly not have been possible without the novel strategies adopted in the consistent fight against polio and other vaccine preventable diseases. We commend the strong domestic and global financing and the commitment of government at all levels,” the Executive Director stated.
Innovation, partnership and resolve have all underpinned advancements made in Nigeria, together with the commitment of tens of thousands of health workers. “Since the last outbreak of wild polio in 2016 in the northeast, Nigeria has strengthened supplementary immunization activities and routine immunization, implemented innovative strategies to vaccinate hard-to-reach children and improved acute flaccid paralysis (AFP) and environmental surveillance. These efforts are all highly commendable,” said WHO’s Officer in Charge for Nigeria, Dr Peter Clement.
However, despite progress, there is still much left to be done. Continued work to reach every last child with the polio vaccine, as well as strengthening surveillance and routine immunization across the region, will be key to keeping wild polio at bay and protecting the gains achieved.
Should there be no more cases in Nigeria or from countries in the Africa Region, and surveillance data submitted by countries meets evaluation criteria, the Africa Regional Certification Committee (ARCC) could certify the Region as wild polio-free as early as mid-2020.
The press briefing was attended by country representatives of all GPEI partners: WHO, UNICEF, CDC, Rotary and the Bill & Melinda Gates Foundation; as well as USAID, Government of Germany, EU and Canada. The Emir of Jiwa, representing the Northern Traditional Leaders Committee was also in attendance.
Read the press release.
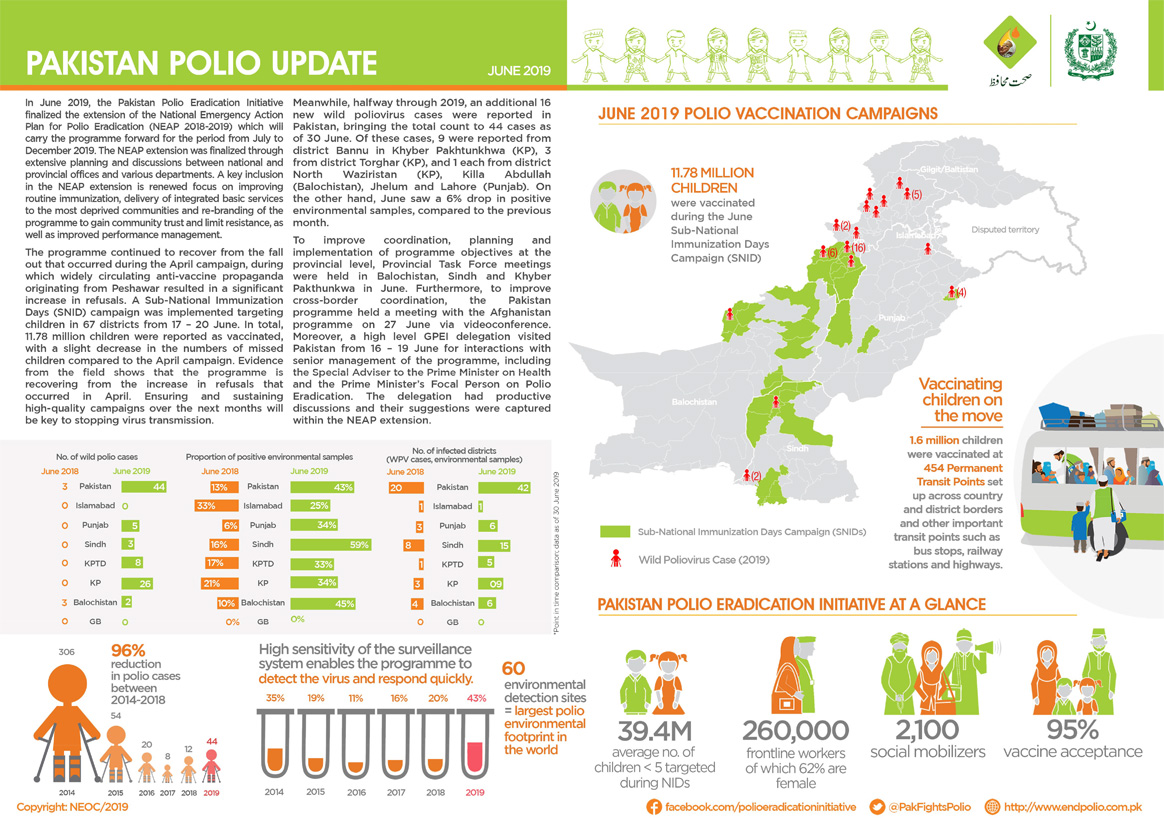
In June:

On the long road to global polio eradication, the programme has achieved four important milestones, representing four out of six WHO regions that have been certified as having interrupted transmission of wild poliovirus (WPVs): Region of the Americas (1994), the Western Pacific Region (2000), the European Region (2002), and the South-East Asia Region (2014).
At present, only the Eastern Mediterranean and African regions— no WPV reported in Africa since 2016, the African region may be eligible for regional certification as early as late 2019—remain to be certified in the path towards global eradication and hence constitute a key priority.
But who decides that a region is free of WPV?
The Eastern Mediterranean Regional Commission for Certification of Poliomyelitis Eradication (ERCC) is an independent body appointed in 1995 by the WHO Regional Director for Eastern Mediterranean to oversee the certification and containment processes in the region. It is the only body with the power to certify the Region free from wild polio, which convenes annually. Here are the outcomes of the recent ERCC meeting:
Urgent need to address regional priorities
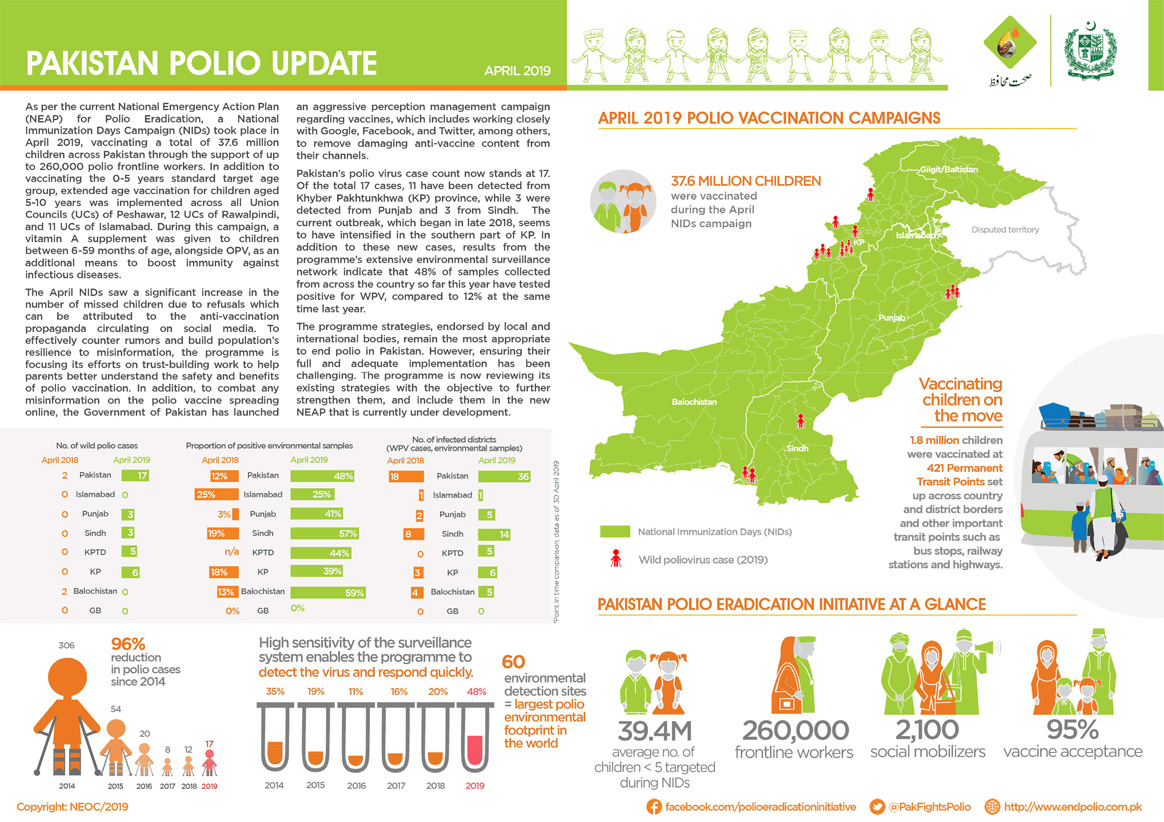
The Commission noted with concern the need to stop the ongoing wild poliovirus type 1 transmission in the only two remaining polio-endemic countries in the Region: Afghanistan and Pakistan. The RCC acknowledged the on-going eradication efforts but strongly recommended the full implementation of the respective national emergency polio programmes through complete political and programmatic support to tackle the WPV1 transmission in the common Pak-Afghan epidemiological corridor, which remains unabated. The Commission also expressed concern about the current circulating vaccine-derived poliovirus type 2 and 3 transmissions in Somalia.
Wild poliovirus type 3 certification prospects
The Commission, however, marked the good progress made towards curbing wild poliovirus type 3 (WPV3). Extensive analyses of the stool and environmental surveillance samples provided evidence that no WPV3 is in transmission in the Region. Based on the epidemiology, EMRO – along with the rest of the world – may be up for global WPV3-free certification by the GCC, potentially certifying two of three poliovirus strains eradicated—WPV2 strain was certified as globally eradicated in 2015.
Stepping-up is the need of the hour
So far, sixty cases of WPV1 are reported from two countries (Pakistan and Afghanistan) in 2019. Given the existing WPV1 transmission in the two remaining endemic countries of the Region, the RCC asked that the Member States undertake a firm commitment necessary for reaching zero.
Eastern Mediterranean Regional Commission for Certification of Polio Eradication (ERCC)
The Thirty-third meeting of the EMRO RCC was held in Muscat, Oman, to discuss the Regional progress towards a polio-free certification. The meeting brought together members of the RCC, chairpersons of the National Certification Committees, polio programme representatives of 21 countries, and WHO staff from the headquarters, regional, and the endemic countries. Representatives from Rotary International and the Centers for Disease Control and Prevention were also in attendance.
Comprised of public health and scientific experts, the regional certification commissions are independent of the WHO and national polio programmes. Global certification will follow the successful certification of all six WHO regions and will be conducted by the Global Certification Committee (GCC).
Final reports of the annual Eastern Mediterranean Regional Certification Commission intercountry meetings.
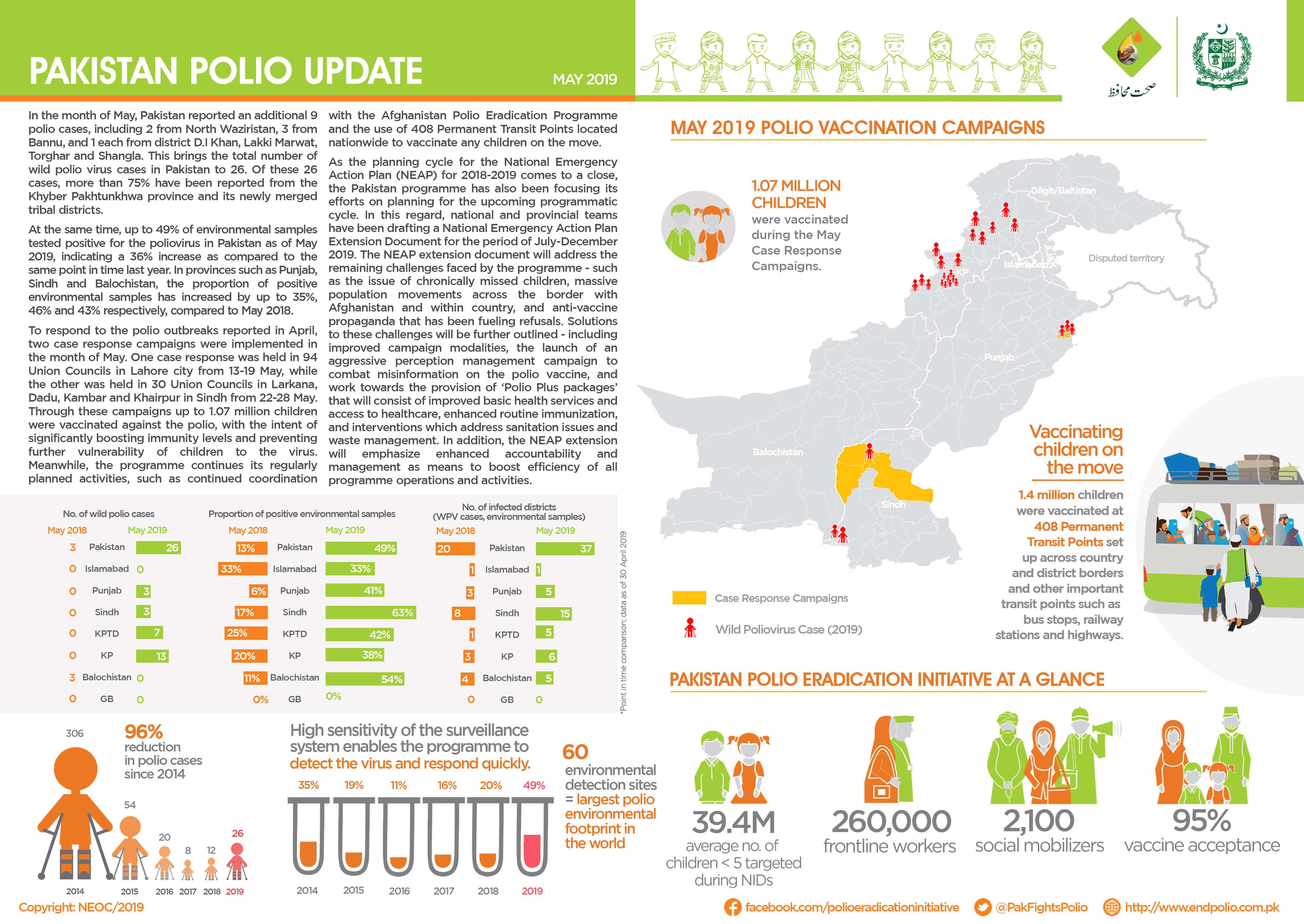
In May
In June

“Our area is a pretty difficult terrain because we live in the water and it is not easy for the teams coming from outside the community to gain access. So, the (hand-drawn) maps make it possible for us to identify areas we have yet to reach during the immunization exercise”, says Peter Idowu, a veteran community mobilizer and team supervisor in Makoko — a riverine shanty town located on the coast of mainland Lagos city, southwest Nigeria. Native to the village, Peter is the man to go to whenever the polio immunization teams face challenges navigating the waterways or the community.

The sprawling water city Makoko is a slum located across the Third Mainland Bridge on the lagoon. It is a largely low-income community with half the population on water and the other half on land. Informal, makeshift houses with corrugated iron roofs sit precariously atop stilts. Down below, narrow wooden boats act as a form of aquatic taxi ferrying goods and people around the bustling community. Nobody knows the exact population of this slum district of Lagos, but it is estimated to be as high as 100 000. It is mostly a fishing community inhabited by the Egun people.
“My goal is to see that all the kids in our community are immunized and live healthy lives. That is why I engage our teams in sensitizing parents all the time on the importance of routine immunization and the dangers of polio. As a member of the community and with a passion of becoming a health worker myself, I kept on mobilizing our people for easy accessibility, because our language is different from Yoruba and most of the Polio teams can’t speak the language. It is always easy with me being in the Polio team as our people will readily accept the vaccine without rejecting,” says Peter.
Nigeria is the only country in Africa and one of the only three in the world endemic to wild poliovirus, alongside Afghanistan and Pakistan. Nigeria is also affected by circulating vaccine-derived poliovirus type 2 (cVDPV2) outbreaks.
UNICEF works closely together with Global Polio Eradication Initiative (GPEI), key polio partners and the Nigerian government. There is a vast network of over 20 000 community mobilizers focusing on demand creation and improving health-seeking behaviors of caregivers.
In May:

“We had not seen vaccination teams in our community for a very long time. Sometimes we go for months without vaccinating our children, if we don’t take our children to the mainland to get them vaccinated”, says Mr. Atebakuro Oton George, a fisherman and father of five, residing in Minibie ward of Nigeria’s Bayelsa State.
A largely riverine state, Bayelsa accounts for over 60% of the delta mangrove of the Niger Delta. Many children here continue to miss their chances at life-saving vaccination, as transport is precarious in the tangle of creeks and rivers that crisscross the state. In 2018 a number of innovative strategies such as, immunization boats at sea and community engagement through the traditional hierarchy and sensitization activities, supported by World Health Organization (WHO) through the Government of Bayelsa were introduced to reach a wider net of children.
“Now on weekly basis, health workers brave the seas and visit our communities to vaccinate our children”, an elated Mr. George continues.
Subsistence farming and fishing are the mainstay of the local population’s economy and diet. Health services are provided by primary health care centers located within the island communities.
“The difficulty of accessing healthcare services is due to suboptimal and expensive coastal and waterway transportation from the distant communities to healthcare centers, hence, innovative strategies are being employed to reach the underserved and vulnerable population with vaccination and other health interventions especially during Supplemental Immunization Activities (SIAs)”, says Dr Edmund Egbe, WHO State Coordinator in Bayelsa.
To reach ‘missed’ children, community engagement activities to increase demand for immunization have been initiated to bolster willingness of caregivers to readily access the interventions even when in the middle of the river or the ocean. The successful implementation of the community engagement framework has resulted in high-level acceptance of immunization services in the State. From April 2018 to April 2019, over 169 836 children received vaccination.

Routine immunization coverage has improved remarkably: the first quarter RI Lot Quality Assurance Survey (LQAS)— a quarterly activity organized by the National Emergency Routine Immunization Coordinator Centre (NERICC) to assess routine immunization performance, reasons for non-immunization as well as efforts to improve uptake and utilization of RI in Nigeria—conducted in April 2019 indicate that the State is second best in the country. Previously, the State was ranked amongst others in the country as poor-performing from the last National Immunization Coverage Survey (NICS) conducted in 2016; this led to the inauguration of an emergency response committee in March 2018.
King Diete-Spiff, the Chairman and the ‘Amanayanbo’ of Town-Brass, in his meeting with the State Traditional Rulers Council said, “Sustaining the innovative strategies of vaccinating vulnerable populations will undoubtedly increase immunity against vaccine preventable diseases and reduce the mortality and morbidity rate in difficult to access communities”. He described the polio infrastructure in Bayelsa, supported by WHO and partners, as the bedrock of driving successful healthcare intervention at the grassroots.
Support for polio eradication and routine immunization to Nigeria through WHO is made possible by funding from the Bill & Melinda Gates Foundation, the Department for International Development (DFID – UK), the European Union, Gavi, the Vaccine Alliance, the Government of Germany through KfW Bank, Global Affairs Canada, the United States Agency for International Development (USAID), Rotary International and the World Bank.
A legion of supporters across neighbourhoods, schools, and households are creating a groundswell of support for one of the most successful and cost-effective health interventions in history: vaccination. These are everyday heroes in Pakistan’s fight against polio.
These thousands of brave individuals are championing polio vaccine within their communities to enlist the majority in the pursuit of protecting the minority — reaching the last 5% of missed children in Pakistan.
One of the major factors that determines whether a child will receive vaccinations is the primary caregiver’s receptiveness to immunization. The decision to vaccinate is a complex interplay of various socio-cultural, religious, and political factors. By educating caregivers and answering their questions, these Vaccine Heroes serve as powerful advocates for vaccination, even creating demand where previously there might have been hesitation. This is where everyday people step in to vouch for vaccination as a basic health right.
Here are some nuanced, powerful, and thought-provoking testimonies on their unwavering belief in reaching every last child:
In April

Polio eradication was in high-level spotlight this week in the top echelons of global leadership as World Health Organization (WHO) Member States, donors, partners, civil society organizations, health and development actors gathered this week at the 72nd World Health Assembly (WHA) in Geneva, Switzerland.
In his opening address to delegates, WHO Director-General and Chair of the Polio Oversight Board (POB), Dr Tedros Adhanom Ghebreyesus talked about the long-winding journey of polio eradication since its adoption as a landmark resolution at the WHA in 1988 and the hopes of finishing eradication in the near future: “Together with our partners at Rotary, CDC, UNICEF, the Bill & Melinda Gates Foundation and Gavi, the Vaccine Alliance in the Global Polio Eradication Initiative, we have launched a new strategy to address the most difficult remaining areas in Afghanistan and Pakistan. Earlier this year I came across a video of a man called Irfanullah, wading through snow to deliver polio vaccines in Pakistan. With the dedication and commitment of people like him, I have no doubt we will succeed in making polio history.”
Member States expressed overwhelming support of the Polio Endgame Strategy 2019-2023. The new strategy sets the stage for a decisive win against polio through the parallel pursuit of the wild poliovirus and circulating vaccine-derived poliovirus. The Strategic Plan incorporates collaboration with other health interventions, fostering stronger alliances and managerial innovations by working in close coordination with governments in endemic countries. The Member States welcomed the trifecta of Eradication, Integration, and Containment/Certification, which set the foundations of a sustainable polio-free world by anchoring polio activities within the broader immunization system, ensuring an effective transition of eradication knowledge and assets and ensuring that no poliovirus can paralyze children again.
With an eye towards an inclusive and sustainable polio-free future, there was broad consensus that all stakeholders—governments, GPEI partners, private and public donors, policy makers, health, and non-health actors— are in this together. One of the recurring themes was the need to ensure concerted efforts—financial and programmatic— to get over the hump in this last mile over to the finish line.
The general air was that of cautious optimism, as all Member States acknowledged that the path to finishing polio eradication is well within sight, all thanks to the Endgame Plan 2013-2018 which succeeded in certifying South-East Asia (SEARO) as polio-free, brought the African Region closer than ever to eradication of wild poliovirus, possibly eradicated two out of three wild poliovirus strains, set the world on the path of phased Oral Polio Vaccine (OPV) removal, stopped outbreaks in Syria and Horn of Africa, and cornered wild poliovirus circulation to a joint cross-border reservoir between Afghanistan and Pakistan.
The delegates particularly appreciated the strong commitments espoused by Afghanistan and Pakistan for a more systematic collaboration to jointly target the common wild poliovirus reservoir on all fronts with an approach that combines the scientific with the social and anthropological. Pakistan’s representative said, “We remain resolute with the highest level of political commitment… strengthening routine immunization, addressing prevalent malnutrition, and provision of safe water and sanitation are strategies being implemented in tandem. Communication challenges of low-risk perception and concerns around vaccine safety and efficacy are being addressed through a revised communication strategy. We continue to coordinate with Afghanistan programme to share experience in strategies to manage the common epidemiological block. In light of the recent cases, the Government of Pakistan has decided to carry out a comprehensive programme review on an urgent footing. I would like to sincerely thank our partners and donors who are a part of this initiative and helped us get this far. We pledge our complete commitment to reach every last child, so no future generations have to suffer from a crippling disease like polio.”
Rotary International, one of the pioneering partners of the GPEI, maintained that wild poliovirus eradication remains the overriding priority, and to that end, re-affirmed collective commitment of their 1.2 million members around the world: “It is easy to forget the hurdles we have overcome—such as: addressing outbreaks in more than 20 countries in Africa, or how India had 80% burden of the total polio caseload in the world. Our challenge is not feasibility, but determination…global commitment has brought us to the threshold of a polio-free world. Let us act with urgency to end polio forever.”
In his closing remarks, Dr Tedros thanked the Crown Prince of Abu Dhabi and the United Arab Emirates for hosting a pledging moment for the Global Polio Eradication Initiative, “Global progress to end polio would not be possible without partners like the UAE. I would like to thank His Highness Sheikh Mohamed bin Zayed Al Nahyan, Crown Prince of Abu Dhabi, and the UAE – a long-time supporter of the polio programme – for agreeing to host the GPEI pledging event this November at the Reaching the Last Mile Forum, a gathering of leaders from across the global health space.”

The 72nd World Health Assembly, the governing body of the World Health Organization held by in Geneva, Switzerland is the biggest congregation of public health actors. Taking advantage of the critical mass of global leaders, the Global Polio Eradication Initiative hosted an event for polio eradicators, partners and stakeholders on 21 May 2019.
The event, To Succeed by 2023—Reaching Every Last Child, celebrated the GPEI’s new Polio Endgame Strategy 2019-2023. The five-year plan spells out the tactics and tools to wipe out the poliovirus from its last remaining reservoirs, including innovative strategies to vaccinate hard-to-reach children and expanded partnerships with the Expanded Programme on Immunization (EPI) community and health emergencies.
The informal event brought together a cross-section of stakeholders – partners, health actors, non-health actors, supporters, donors, Ministers of Health of endemic countries, WHO Regional Director for the Eastern Mediterranean, and Polio Oversight Board members – alluding to strengthened and systematic collaboration in areas of management, research and financing activities in the last mile.

Dr Zafar Mirza, Pakistan’s Minister of State,Ministry of National Health Services, Regulations and Coordination, took the stage and gave insight into country-level polio eradication efforts and the need for coordinated action with Afghanistan: “20 years ago, 30 000 children were paralyzed by polio in Pakistan. This year, 15 cases have been reported. While we have done a lot, it is clearly not enough. We are resolute in this conviction. We, together with Afghanistan, must make sure we eradicate polio for the sake of our children. Our science is complete, only our efforts are lacking. Along with the polio programme, the donors and the Afghan government, we will get to the finish line.”
Echoing similar sentiments, Dr Ferozuddin Feroz, Minister of Public Health of Afghanistan, said, “I would like to start by expressing thanks to all the partners for their support. As you know, Afghanistan has a very challenging context due to inaccessibility, refusals, gaps in campaign quality, low routine immunization coverage, and extensive cross-border movement. But, Afghanistan has made progress—five out of seven regions continue to maintain immunization activities. We view polio as a neutral issue and have developed a robust National Emergency Action Plan 2019. We appreciate the Polio Endgame Strategy 2019-2023. We believe coordination with Pakistan will help us deliver a polio-free world. We look forward to your continued technical and financial support to achieve the goal of polio eradication.”

Recognizing the long-standing commitment of the United Arab Emirates, a video was played showing the on-ground efforts of the Emirates Polio Campaign, working with communities and families in Pakistan in collaboration with the Global Polio Eradication Initiative and partners, and the Government of Pakistan. Thanks to the Emirates Polio Campaign, 71 million Pakistani children have been reached with 410 million doses of polio vaccine.
Dr Abdullahi Garba, Director for Planning, Research and Statistics, National Primary Healthcare Development Agency spoke on behalf of Professor Isaac F Adewole, Federal Minister of Health of Nigeria. Dr Garba harked back to the past as the GPEI plans for the future: “Nigeria started actively working to eradicate polio in 1988, at a time when we used to have up to a thousand cases every year. With all our innovation and efforts, I am pleased to inform you today that no wild polio case has been detected for the past 33 months. This feat was achieved through continuous efforts between the government, GPEI and partners, having diligent incidence reporting, reaching inaccessible children, and improving the quality of the polio surveillance immunization activities through strong oversight mechanisms in Nigeria. I know I also speak on behalf of all countries across Africa – we will achieve success.”

Rounding off the evening, Dr Tedros Adhanom Ghebreyesus, the World Health Organization Director-General and Chair of the GPEI Polio Oversight Board, took the stage to recount his first visit of the year to the polio endemic countries of Afghanistan and Pakistan, the progress made over decades, and the need to re-commit to the cause of ending polio. “Together with Regional Director Ahmed Al-Mandhari and Chris Elias of the Gates Foundation, we travelled to Pakistan and Afghanistan. We saw first-hand the commitments by both public and civil society leaders, which gave us a lot of confidence. The other thing that gave us confidence was seeing our brave health workers trudging through deep snow. And of course, our partners: Rotary, United Arab Emirates, CDC, UNICEF, the Bill & Melinda Gates Foundation and Gavi. The last 30 years have brought us to the threshold of being polio-free…(which) lay out the roadmap that is the Polio Endgame Strategy 2019-2023. The Ministers of Afghanistan and Pakistan have also assured us that they will continue to work together in their shared corridor to finish polio once and for all.”

In 1988, the World Health Assembly passed a resolution to globally eradicate poliovirus, in what was meant to be “an appropriate gift…from the twentieth to the twenty-first century.”
As the GPEI plans for the future and its final push to ‘finish the job,’ it is clear that political and financial efforts need to ramp up in this increasingly steep last mile. As he concluded, Dr Tedros thanked committed partners like United Arab Emirates: “Global progress to end polio would not be possible without partners like the UAE. I would like to thank His Highness Sheikh Mohamed bin Zayed Al Nahyan, Crown Prince of Abu Dhabi, and the UAE – a long-time supporter of the polio programme – for agreeing to host the GPEI pledging event this November at the Reaching the Last Mile Forum, a gathering of leaders from across the global health space held once every two years…let us join together to end polio.”