Steve Oberste has been chief of US CDC’s picornavirus laboratory since 2012. He also worked as a research microbiologist at CDC, from 1996 – 2011.
Could you please provide some background on your labs and the polio-related work carried out there?
SO: CDC’s polio and picornavirus lab is a global specialized laboratory in the WHO Global Polio Laboratory Network. It was set up in the mid-1950s and is US-government funded, with CDC being an agency under the Department of Health and Human Services. Our polio lab is one of the largest out there with approximately 55 staff dedicated to polio. We largely deal with the more complex side of polio diagnostics – sequencing, which is the molecular testing of poliovirus-positive samples to determine genetic connections to other known polioviruses.
We also act as a ‘lab of last resort’ when countries, for whatever reason, are unable to carry out preliminary diagnostic tests on their samples. We’re involved in the development of a new and even safer form of oral polio vaccine, and have a team which looks at population immunity through examining blood samples from communities (serosurveys). Importantly, we also develop and distribute reagent kits for testing samples for polio, to labs across the Network.
PB: The polio laboratory at KEMRI is combined with the measles and rubella laboratory and has been in operation since the 1980s under the general virology programme. The lab became formally accredited as one of the WHO Global Polio Laboratory Network labs in 2000. Our primary role in relation to polio is supporting surveillance through detection, i.e. isolation of poliovirus from samples we receive. We also conduct intratypic differentiation to identify strains of polioviruses isolated. KEMRI has 12 staff working on polio. WHO funds our routine diagnostic work and supplies and the Kenyan government funds our infrastructure, staff and recurrent costs such as electricity.
What’s the geographic scope of the support you provide?
SO: CDC’s polio lab provides sequencing support to countries around the world. Some examples of countries we are currently assisting include Nigeria, Yemen and those in the Horn of Africa. In terms of serosurveys, we’ve recently done work for Nigeria, DR Congo, Sri Lanka, Ukraine, Pakistan and Lebanon to name a few. We also assisted with testing of samples from Syria during recent polio outbreaks.
PB: We test samples collected from Kenya, Somalia, Djibouti, Eritrea and occasionally from Yemen, for poliovirus. In a year, we would process roughly 4,000 samples and we’ve tested about 200 from Yemen this year. In fact, around 800 samples from Yemen arrived just yesterday. We are in the process of shipping these on to CDC in Atlanta as currently we do not have the capacity to test this quantity. We assist when we can but need to be careful of our capacity so we don’t compromise our support to the other countries.
Type 2 poliovirus (PV2) has been eradicated and WHO has called for countries to destroy unneeded PV2 stocks. However, some will continue to keep PV2 to perform critical functions. Facilities keeping the virus will need to follow GAPIII guidance and pass through a rigorous certification process to prove they can safely and securely handle and store the virus. Their governments are also responsible for putting in place safeguards to minimize risk of containment failure. CDC has decided that it will continue to work with poliovirus but KEMRI has decided to destroy its infectious materials. How were these decisions made?
Dr Peter Borus has been at KEMRI since 1994. Before moving to polio, he worked in yellow fever serology and virus isolation.
SO: To do the diagnostics and research work we do, it’s a basic requirement to have a large bank of samples of known identity – PV2 or otherwise. We also need samples to produce our kits, which we distribute to around 120/146 of the Network labs worldwide. CDC has been involved in containment for about 15 years and so understands the GAPIII requirements very well. Most of our facilities meet specifications although a few modifications are needed.
The bulk of the work ahead is related to work practices and documentation ‒ essentially making sure all our i’s are dotted and t’s are crossed. We’re bringing on a containment and safety manager to help with this and with monitoring and training. CDC is also looking closely at its risk assessment models and revising protocols for use in the event of a spill.
PB: Initially, we oriented ourselves to what it means to go through this process and become a poliovirus-essential facility (PEF). We looked at costs; actually the major determinant behind the decision was cost.
The costs of maintaining the infrastructure necessary to remain a poliovirus-essential facility are not tenable as the resource demands are above the government’s capacity. The decision was not from a lab safety aspect. We operate on biosafety level 2 and are a low-risk facility from our own assessments. However, the demands of GAPIII include certain other safeguards.
The primary safeguards that we have here we could easily manage, but the secondary and tertiary safeguards including immunization of the surrounding community and high levels of immunity, the requirement for an effluent system going out of our lab… these are things that made it [becoming a PEF] untenable for us as a country to maintain. In view of the implications of resources versus the benefits, the Kenyan government decided it was not worth KEMRI becoming a PEF.
What were the arguments, if any, for keeping samples at KEMRI?
PB: As any researcher would know, the material is valuable. That was the main argument for retaining. We refer to our stool sample collection as ‘golden stool’ ‒ golden because samples really generate information. When you have isolates, these are useful to share with other facilities on request for vaccine production.
For the unprocessed samples which contain poliovirus, as a research institution, this material is very useful to us for diagnosis of other agents. But when you look at it from the perspective of committing a whole country to putting a lot of resources in [to become a PEF], you say ‘OK, fine’. You let go.
What process did KEMRI follow to destroy its infectious material? And what happens to the new positive samples that come in?
PB: We had a local containment committee in-country who oversaw the destruction activities. We had an inventory and they set a date for us. We removed all our archived wild virus materials from storage and put them in an autoclave. So it was heat deactivation; we incinerated all the materials. KEMRI management and government officials witnessed the process. Because of the large amount of archived materials, it took one full week to prepare and actual destruction took three days. We didn’t want to come back and repeat the process for types 1 and 3 materials and so destroyed all types 1, 2 and 3 wild virus materials at the same time.

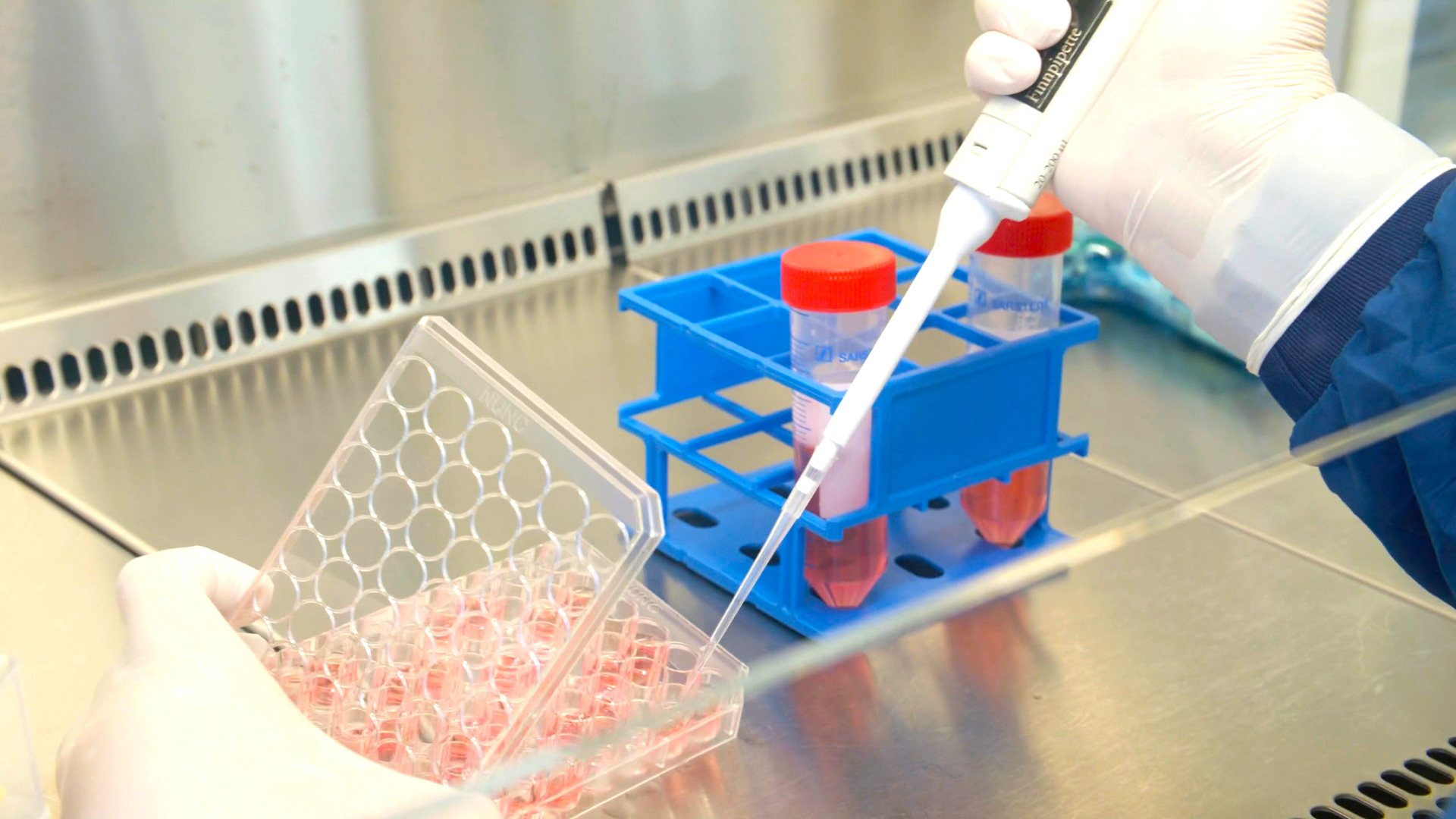
CDC scientist Chelsea Harrington placing samples into a real-time thermocycler, to identify the various types of poliovirus contained therein.
For new samples, we archive those positive for types 1 and 3. For type 2, all isolates are sent to CDC for sequencing and original stools are destroyed within 72 hours of the final genomic sequence result.
Having experience with containment, does CDC’s polio lab help others reduce risk of breaches?
SO: We help answer technical questions coming from other facilities in the US looking to contain the virus. Part of preparing to become a PEF is to have emergency plans in place in case there is a spill. We assist facilities in putting together their plans, and can help out with response if there is a spill.