In March:
- No case of WPV1 was confirmed
- 37.7 children under the age of five were vaccinated during the March National Immunisation Days (NIDs)
In March:

Dr Hamid Jafari, Director of Polio Eradication for WHO’s Eastern Mediterranean Region, declared Somalia’s outbreak of circulating vaccine-derived poliovirus type 3 (cVDPV3) closed a full 28 months after this strain of polio was last detected in Somalia.
Seven children were paralysed by the type 3 strain in the 2018 outbreak, and sewage samples regularly monitored for poliovirus tested positive for cVDPV3 a dozen times, beginning March 2018. There is no doubt that the virus circulated widely around southern and central Somalia. Despite extensive disease surveillance measures, no cVDPV3 has been identified since 7 September 2018, when the last child developed paralysis.
Closing a polio outbreak is a formal process steered by a detailed checklist of surveillance indicators that must be met in order to show that the virus is not just hiding in a far-flung pocket but has truly disappeared. Sewage runoff is tested for virus, and health workers and community members actively search for paralysis in children, and then investigate any paralysis they do find to rule out polio. Accessing hard-to-reach communities is a challenge in Somalia, but a vital aspect of this work.
The 2018 cVDPV3 outbreak was part of a 2-strain polio outbreak in Somalia at that time, along with circulating vaccine-derived poliovirus type 2. Both strains emerge and paralyse children in under-immunized populations – places where not enough children have consistently had access to polio vaccines. The cVDPV2 outbreak continues to paralyse children, and environmental samples – sewage water – consistently show that virus moving through Somali communities. For the polio programme, the presence of cVDPV2 samples and the absence of cVDPV3 samples is bittersweet: it demonstrates the sensitivity of our testing, so we can be confident cVDPV3 is no longer a threat to Somali children – but it makes clear that the threat of paralytic polio still looms.
Across the Region, cVDPV2 cases are on the rise – as across much of WHO’s African Region. Wild poliovirus still stalks children across Afghanistan and Pakistan, and the movement of people across borders underscores the risk of importation across and beyond the Region.
The end of Somalia’s cVDPV3 outbreak shows what can be achieved with high-quality vaccination campaigns, on-the-ground leadership and sensitive surveillance measures.
In his English writing class, Mujahid Miran was asked to write an essay titled the “Aim of life”. This was a space for the students to imagine who they could be and what they saw themselves as when they grew up.
Miran wanted to be a captain in the army and he eagerly shared this ‘aim of life’ in his essay. After his hopes made it to the page, his teacher immediately shot it down: There was no way he would make it, she told him, because he had polio.
Born in 1985, Miran grew up in Kohat and contracted polio when he was two. This was a year before the Global Polio Eradication Initiative was founded in 1988, leading to a worldwide vaccination campaign to fight the spread of the disease. In the decade of the ’80s, the estimated number of cases was over 350 000 per year, while the disease was still prevalent in 125 countries. With focused efforts around the world to eradicate the poliovirus, the number of paralytic cases was reduced by 99.99% with 42 cases in 2016.
For Miran, school was among the most challenging periods of his life. “School life was generally very hard. It must be easier for polio survivors to study in special schools, but in a usual school, I was always referred to as langra, mazoor (derogatory words in Urdu for people with disabilities). I was always made to feel different.”
The challenges were frequent, never letting him forget that he couldn’t walk from one leg. “Among the things that would hurt a lot was sports class or recess. “Every time kids would be chosen for a sports activity, I was completely sidelined – as if I wasn’t even there.” he says.
Academically, Miran always performed well in class and would usually be among the top three students. I always had among the best grades, but I would never be nominated to be the class monitor or get a position as part of the student council, he says. “Every week I’d go to my teacher and ask her why I was never nominated because other students who would be poorer than me academically would be chosen instead. A part of me knew even back then that it was my disability, but now looking back, I know it was exactly that.”
After having lived with polio for 33 years now, Miran is now based in Karachi and is part of a small seafood export business. He buys seafood from factories in Pakistan to sell in southeast Asia and makes an income for the commission he makes per sale.
Miran is able to independently support his family of his wife and two children, aged six and two, but the everyday realities of living with polio make the smallest of tasks harder.
“There is such little awareness in Pakistan, and it’s even within government institutions. I had to get my special driver’s license and when I went to get it made, the officer on duty asked me to raise my shalwar in front of a group of people and stand on one foot to prove I had a disability, he adds. “The humiliation is too much.”
This virus has also been an obstacle in maintaining friendships, as most places for leisure in Pakistan have no access for people with disabilities. “Plus, there is also so much shame in it. I was in Dubai once and I was walking with a friend who turned around to me and said that the way I was walking was embarrassing for him. This virus impacts your life in every way.”
Last year, Africa was declared wild polio-free after Nigeria, the last remaining country in the region that had polio and accounted for more than half of all global cases less than a decade ago, had no cases of wild poliovirus for the fourth year running.
Today, Pakistan and Afghanistan are the only two endemic countries in the world and global efforts continue to vaccine children in this epidemiological block, and finally make the dream of a polio-free world possible.
Miran says this interview is his personal effort to spread awareness on polio. “I talk to everyone in my friends and family circle who have young children. I give them my example and tell them they can’t afford to miss out on vaccination. I am very regular with my children’s vaccination too. Whenever polio teams come to our house, I make sure the children take polio drops.”
At many times in the interview, Miran mentions how the physical pain caused by the disease is often unbearable. “I almost never express how much pain I feel because people will think I’m asking them for financial help or wanting their sympathy. But I just want everyone to know that living with polio is hard. Very, very hard.”

Therese and Léonie reminded me of this hard truth in a recent visit to a hospital in N’Djaména, Chad. One is a newborn girl and the other is a veteran of the campaign to eradicate a human disease for only the second time in history –polio-.
As a Gender Champion for Polio Eradication, I have committed to supporting the global initiative to eradicate polio and the women who work tirelessly to protect children from lifelong paralysis. During my visit to Chad, I had the honour of giving two drops of life-saving oral polio vaccine to two newborns.
Protected from a disease which once struck millions of children, Therese now has a better chance of a healthy life. Thanks to the Global Polio Eradication Initiative (GPEI) – spearheaded by Rotary International, national governments, the World Health Organization, UNICEF, CDC, the Bill & Melinda Gates Foundation and Gavi, the Vaccine Alliance – she is one of more than 2.5 billion children who have received the oral polio vaccine, as the global polio caseload has been reduced by 99% since 1988.
But as I looked at Therese, I also wished that she would have a better chance not just for health, but also for opportunities to prosper. I thought of a recent WHO report I had read – Delivered by Women, Led by Men – which observed that women make up 70% of the global health workforce but hold only 25% of senior roles – a situation that is no different for the polio program. Would Therese’s future reflect that disparity?

I found both frustration and hope in answer to my question when I listened to Ms. Léonie Ngaordoum, the woman responsible for the campaign which brought the vaccine to Therese.
Léonie is head of vaccine operations for Chad’s immunization programme. It is women like her who have brought us this far in the long fight against polio. It is women like her who have gone the extra mile to keep their countries safe when, in 2020, the polio programme faced unprecedented challenges in the face of a new pandemic- COVID-19.
Her journey to a senior public health position in Chad has been difficult. Driven to remote areas on dangerous roads to oversee vaccination campaigns, she has twice suffered accidents, one of which left her with severe spinal injuries. She has faced gender discrimination, countered vaccine misinformation, convinced vaccine sceptics, and stayed the course despite the severe strain of COVID-19, and struggling for respect and recognition in a male-dominated environment.
Today she has a clear vision to share: “I speak about vaccination as if it were a vocation…the program change needed to achieve polio eradication is to empower enough women.” Léonie’s experience highlights the necessity of increasing senior roles among women in the health workforce and involving them in policy decisions.
Women like her frequently operate in dangerous and conflict-affected areas, putting their own personal safety at risk – all in efforts to protect communities from deadly diseases. Women have a greater level of trust with other women and thus are able to enter households and have interactions with mothers and children necessary to deliver the polio vaccine. And this way they can also provide other services, such as health education, antenatal care, routine immunization, and maternal health.

The knowledge and skills gained by this workforce are already being deployed against COVID-19, in surveillance, contact tracing, and raising public awareness. Indeed, more than 50 percent of the time spent by GPEI health workers is already dedicated to diseases and threats beyond polio. It’s clear that the future of public health is inextricably linked to the status of women. Their heroic actions provide nothing less than a blueprint for the future of disease prevention. The Resolution on “Women, girls and the response to COVID-19”, adopted last year by the UN General Assembly, should play a key role when addressing these challenges and the specific needs of women and girls in conflict situations.
The centrality of women to the success of public health projects has for too long gone unrecognised, and must be formalized. That is why today, on International Women’s Day, we must pay tribute to the tremendous contribution of women like Léonie around the world in protecting their communities from deadly diseases such as polio. But at the same time, thinking of the world in which Therese will come of age, we need to commit to empower every woman and girl. It will not only make for a more just world – but a healthier one too.

From her first polio vaccination campaign in 1997 to the present day, Dr. De Sousa has never lost her passion for increasing access to immunization. The National Expanded Program on Immunization (EPI) Manager for Angola, she remembers her first impressions of the country, “At the time, I could see that most children in the country were not vaccinated and I was excited to help them.”
From the outset, she knew that taking on polio eradication would be challenging. “Angola had just emerged from an armed conflict and there were areas that were very difficult to access, due to dilapidated roads, broken bridges and mining activity, and for that reason there was low routine vaccination coverage. Nevertheless, I felt that I had a duty to fulfill for our children, so I accepted the challenge.”
In 1998, Dr. De Sousa was appointed by the National Directorate of Public Health to help implement the Epidemiological Surveillance System for Acute Flaccid Paralysis (AFP) – one of the primary symptoms of polio. It was a position that required grit and resilience.
She explains, “This was a big responsibility because highly sensitive surveillance for AFP, including immediate case investigation and specimen collection, are critical for the detection of wild poliovirus. AFP surveillance is also critical for documenting the absence of poliovirus circulation for polio-free certification.”

“One of my most vivid memories of the programme is from 1999 when I was trying to reach conflict-affected areas after a polio epidemic had registered more than 1190 cases and 113 deaths. I was early in my career with only two years of service and the sheer number of cases and deaths led me to be proactive and persistent in my day-to-day activities toward the eradication of the disease.”
“Another standout moment occurred on the second time that I went to coordinate a vaccination campaign in the province of Moxico; one of the vehicles in our convoy triggered a mine, so we were forced to stop the vaccination campaign as our colleagues were stranded in conflict zones for a few days. This incident captures the difficult circumstances we were operating in as health workers.”
Eradicating wild virus in Angola
For years the polio team worked to improve operations to detect polio and deliver vaccines, but the virus fought back. After registering a last case of indigenous wild poliovirus in September 2001, Angola recorded four successive outbreaks imported from India and Congo. Dr. De Sousa remembers that this caused many people to doubt that the eradication of polio would ever be possible.
“But I refused to be discouraged. I’ve never backed down from a challenge and I don’t plan to soon.”
After years of work, Angola finally received wild polio-free status in November 2015. Dr. De Sousa describes it as her proudest moment.
“I felt that I made a great contribution to my country and our children as the person managing the Extended Program on Immunization in Angola.”
A new challenge
In 2019, Angola’s immunization team faced a new challenge when the polio programme detected an outbreak of circulating vaccine-derived polio type 2, a type of polio that emerges in places with low immunity. Dr. De Sousa again found herself at the forefront of the action, starting by supporting the Government to respond with vaccination campaigns.
One of her key tasks since has been recruiting new immunization health professionals, who can help reach the children missed by routine immunization and polio campaigns. She explains, “my goal is to train my colleagues so that we can work together to reach the vast number of Angolan children missing out on lifesaving vaccines.”
In July 2020, Angola held its first polio campaign after a pause on vaccination activities in the early months of the COVID-19 pandemic. More than 1.2 million children were reached by over 4000 vaccinators.
Gender and leadership
Dr. De Sousa explains that being a woman leader in Angola isn’t easy. “It requires a lot of time, dedication and a balance with domestic, family, and social life, which has not been easy to manage. However, with the help of God and my family – especially my husband – I am managing to carry out my work.”
“It has all been worth it for the results I’ve helped to achieve, and even though we have some way to go in relation to vaccination coverage, I’m grateful for the opportunity to ensure the health of our children and serve my country.”
In Angola, at the provincial and municipal level, there are very few women compared to men. However, in public health programmes at the national level, women outnumber men. Dr. De Sousa says that, “In general, I think there should be more women leading and administering vaccination programmes”.
In 2021, the polio programme is aiming to implement more outbreak response vaccination rounds to reach children with low immunity to the poliovirus. Driven by her passion and sense of duty, Dr. De Sousa will continue to be on the frontlines of this effort.
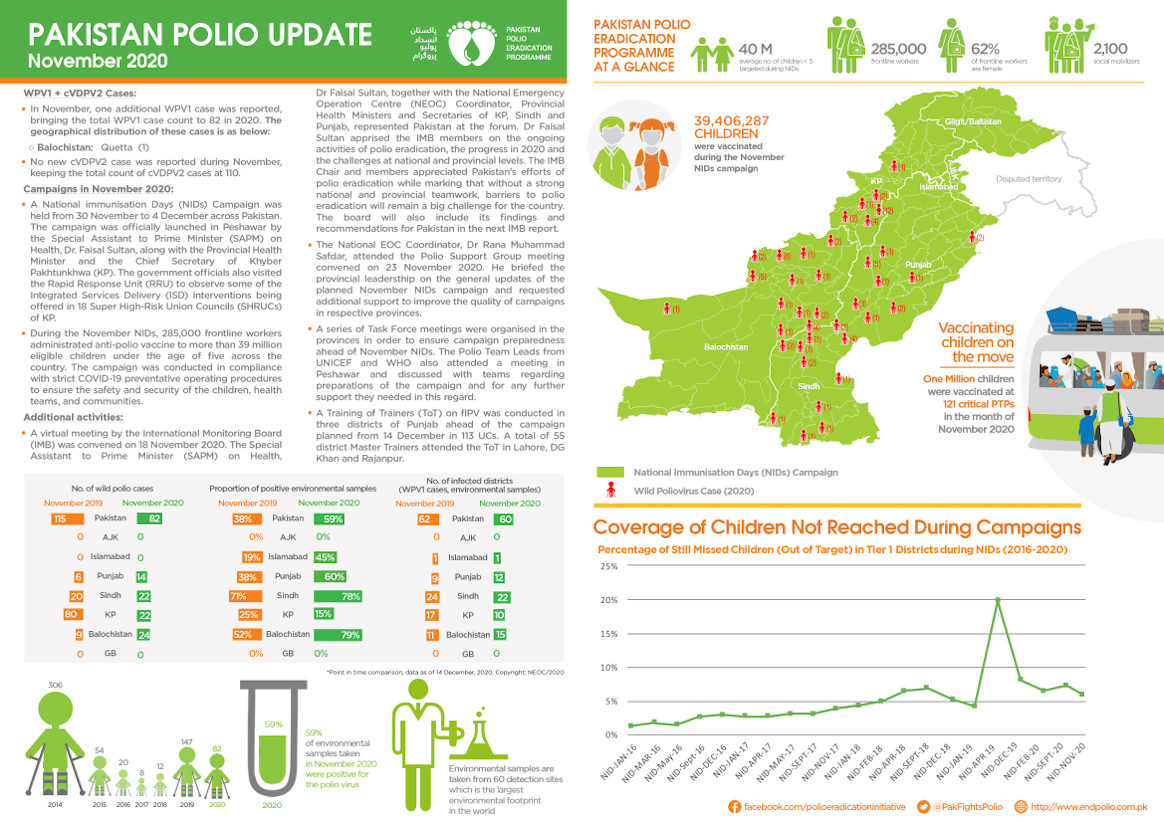
In November:

With masks on their faces and sanitizers in their pockets, an immunization team makes their way through the narrow lanes of Lahore’s historic old city.
“Our children are like flowers and these anti-polio drives help them grow up healthy and strong,” says Zubair, who along with his colleague Afzal is part of Pakistan’s 260,000-strong frontline vaccinator workforce.
It is the second day of the National Immunization Days (NID) campaign, which launched on 21 September, and the third immunization drive after a four-month suspension of door-to door campaigns due to the risks associated with COVID-19.
After polio campaigns were stopped in March 2020, the number of polio cases in Pakistan continued to increase. An initial small-scale round of vaccinations resumed in July, when over 700,000 children were reached. A second round went ahead in August, where 32 million children were vaccinated across the country. In both campaigns, vaccinators took precautions to prevent the spread of COVID-19, including wearing masks and regularly washing hands.
Making their way from the crowded streets of Taxila Gate, the polio team reaches a historic cultural hub of Lahore city called Heera Mandi.
In this neighbourhood, the team knocks on one door after another. “Sister, do you have children under five at home?”, they say.
When the answer is yes, one of the vaccinators stands to the side while Zubair hands them a hand sanitizer. They all stand at a safe distance from each other, to remain compliant with COVID-19 safety measures, and to make sure the dual message of the necessary fight against both polio and COVID-19 reaches home.

Zubair says that since the resumption of immunization campaigns in Pakistan, parents have been more enthusiastic to ensure their children are vaccinated.
Next door, a Maulana (a religious cleric) answers. When he sees the polio team, he immediately goes back inside. Team members worry that he may reject the vaccine, but soon enough, he returns with his two children.
“Did you ever believe that the polio vaccination was a conspiracy?,” the Maulana is asked. In some parts of Pakistan, false rumours about the vaccine have damaged confidence in immunization, with sometimes devastating results for children subsequently infected with polio.
“No Sir, only a fool can think like that,” he replies.
Afzal, another member of the immunization team, says that he finds his work fulfilling because it allows him to directly speak to parents about polio and explain that they can give their children a healthy future by vaccinating them.
With a physical disability, Afzal often faces discrimination based on his health condition. He explains that this hasn’t prevent him from pursuing his ambitions.
“I never allowed my disability to become an obstacle. I completed my master’s degree while attending regular classes at college, and now I have been working with the polio programme for nine years.”
“If a family is hesitant during a polio campaign, I approach the parents,” he says. “I show the parents my polio-affected leg and ask them if they really want their child to have one too. This changes hesitation to acceptance.”
Health workers like Zubair and Azfal are working every day to achieve the dream of ending polio in Pakistan. With their effort and the efforts of thousands like them, the September campaign successfully reached over 39 million children across the country. These promising results, achieved during a pandemic, are a testament to an ongoing commitment to overcome challenges and move Pakistan closer to a polio-free future.
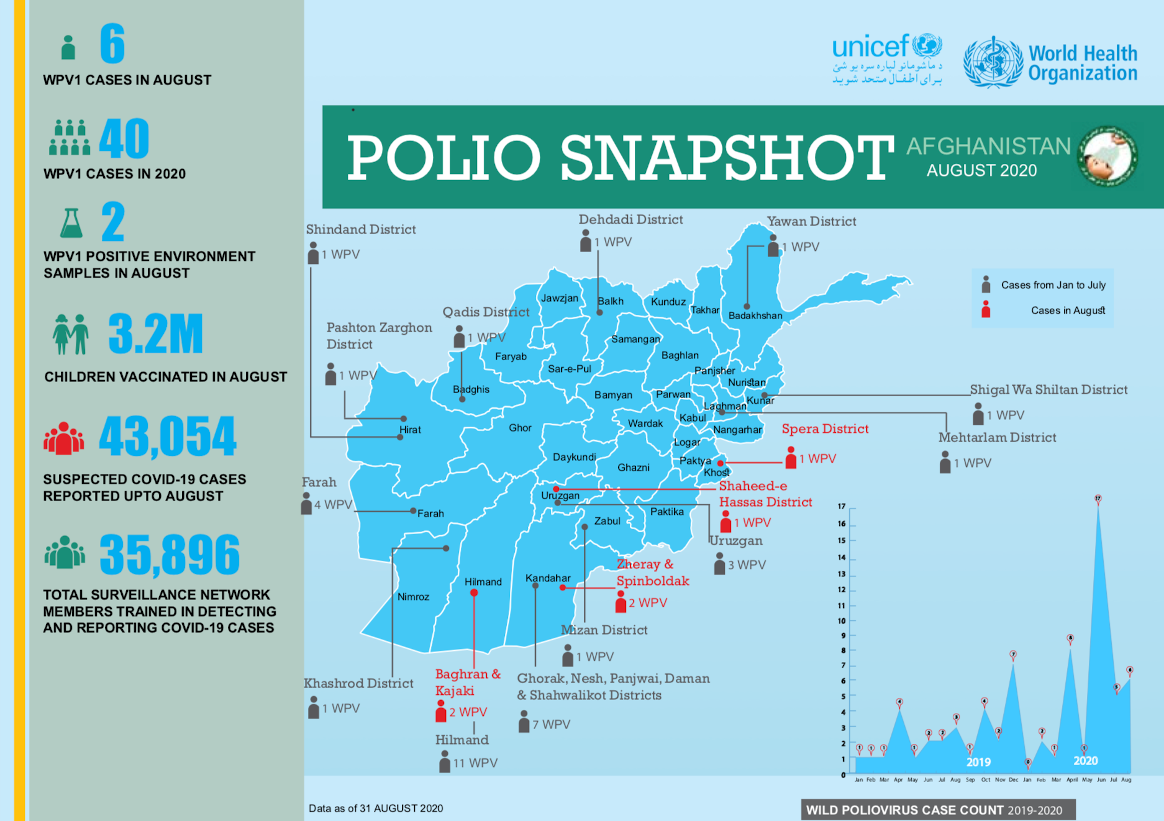
In August:

Dr Elaha, at 22 years old, is a medical graduate and a District Polio Officer. She’s also helping fight the COVID-19 pandemic in Afghanistan.
“COVID-19 has affected both our work life and personal life. When I joined the polio team, I had plans to take initiative and look for innovative ways to fight polio, however, with the COVID-19 pandemic all my plans were challenged,” she says. “Campaigns were postponed and the number of cases were on the rise.”
The temporary pause in polio vaccination campaigns, necessary to keep health workers and communities safe during the early months of the pandemic, led to a widened immunity gap in both Afghanistan and Pakistan, the only two countries that still harbour wild poliovirus. Now, polio teams are urgently working to close the gap while continuing their support to Afghanistan’s COVID-19 response. To ensure their safety, all polio personnel have been trained to take precautionary measures against COVID-19, including wearing masks correctly and regular handwashing.
Dr Elaha doesn’t underestimate the danger of her work to fight COVID-19. She explains, “I start my day at 8am by visiting private and public clinics, pharmacies, traditional healers at their homes. Of course, I am worried about myself and my family getting COVID-19. My mother is elderly, and COVID-19 can be dangerous for her.”
“However, I am committed to serve my people and go out in the field to help save others’ lives. It is not easy. My family understand that I am a medical doctor, so no matter what virus is there, I have to do my job as a doctor.”

Through her work, Dr Elaha has come up against rumours and misinformation. A major part of both ending polio and fighting COVID-19 is working to inform and build trust with communities about diseases and how they can be prevented.
Elaha says, “A lot of people thought that COVID-19 was a disease of nonbelievers. At first, when I used to go to clinics, because of my medical degree, they respectfully listened to me. However, when I talked about COVID-19 and washing hands and other preventative methods, they would tell me that this disease was for nonbelievers.”
“Unfortunately, a lot of people got sick and many also lost their lives. People have started to believe the pandemic. They know that people can get sick and die of the disease.”
Although public awareness about the dangers of COVID-19 has improved, Dr Elaha believes there is still plenty to do to encourage communities to adopt disease prevention measures such as widespread mask wearing.
Until the pandemic is over, she is determined to work long hours to fight both polio and COVID-19. The polio workforce currently contributing to COVID-19 response includes almost 36,000 members of the Polio Surveillance Network, and over 47,000 polio frontline workers.
In August

Welcome to Pehlwan Goth, Pakistan. A low-income neighbourhood on the edge of Karachi city, it is home to many families from Khyber Pakhtunkhwa province who have moved here for work.
An open sewage drain lined with litter runs the length of the settlement. Cattle are often seen grazing near the heaps of garbage. It is a high-risk area for polio, and virus is regularly detected in the environment.
Samreen, a 25-year-old Polio Area Supervisor, leads a team of four community health workers in the area.
“I started working with the Polio Eradication Programme four years ago and I am happy to say that we have made a lot of progress here. This is my neighbourhood; this is where I grew up and this helps me immensely. People here listen to me, especially the women, and I know most of the children by name,” says Samreen.
There are around 32,000 children under five years of age in Pehlwan Goth. In April 2019, parents of around 3,000 children refused the polio vaccine. Through the hard work of supervisors like Samreen however, now over 80% of these children have received vaccines.
“I am in charge of an area that has 210 households with 196 children. In 2019, families of more than 50 children refused vaccines. That’s almost one fourth of all the children in my area,” said Samreen.

“Building trust takes time, and we continued engaging with community members, visiting families, listening to their concerns, and explaining the benefits of vaccination. Today, we have only eight refusal cases out of the previous 50. I will try my level best to bring this number down to zero during the polio campaign next month.”
“But for me, it is not just about just converting refusals during every campaign, I want all families to understand the benefits of vaccines in the long run and ensure the immunization of their children against polio and other diseases.”
Her rapport with families is apparent during house visits. A family with three children, who had refused vaccination in previous months, agreed that their children could this time receive the life-saving polio drops.
Confronting misconception
Building trust with the community has not been an easy task. Samreen is supported by a social mobilizer as well as a local religious support person. The team members work together to address misconceptions and raise awareness of good health practices among caregivers in Pehlwan Goth.

“We speak the same language and our homes are in the same area where we work. It is easier to communicate with people when you are part of the same community,” said Maulana Mohammad Hanif, the religious support person in Samreen’s team.
Sometimes, however, it can take only one negative social media video or news item to reignite refusals and overturn all their efforts.
“The process takes time. The work is tough but I am grateful to Allah for this job, which allows me to feed my family, and contribute to a noble cause, which will save future generations of Pakistanis,” added Maulana Mohammad Hanif.
It’s clear that Samreen and her team will do whatever it takes to deliver a polio-free future to all 196 children in their care. Pakistan and Afghanistan are the final two polio endemic countries in the world and there are still many challenges that remain.
It is the local efforts of teams like Samreen’s that will make all the difference – by listening to communities, building trust and ensuring rapport, they are playing a crucial role to bring their country closer to ending polio.

In March 2020, polio social mobilisers from the UNICEF-run Immunization Communication Network (ICN) provided routine immunization referral services to over 37,000 children in southern and eastern Afghanistan.
The polio programme’s routine immunization efforts in Afghanistan have made important gains, especially in the country’s east, in the areas bordering Pakistan. Polio social mobilisers support mother and child health referral services, and help families keep track of their children’s health records. As the mobilisers are recruited from their community, they know the families in their neighborhood and can trace each child’s planned immunization schedule from birth.
It is critical that routine immunization continues throughout the pandemic to protect children from life-threatening diseases including polio. Polio mobilisers have found their work is even more valued during the COVID-19 response.
Masoud, a polio mobiliser, says ‘’I used to announce the immunization sessions through the Mosque but not all the targeted children were brought to the health facility. Now through the ICN support to routine immunization, the number of missed children has reduced due to tracking of every child in the community and coordinating with the health facility.”
“This is critical during the ongoing pandemic, as families are not sure if they can leave their homes to take their children to the health facility for immunization. The polio mobilisers are their guide in the community.’’
Part of Joana’s role as a nurse involves vaccinating children in Barangay 105 Happyland, Tondo, in the city of Manila. A vaccine-derived poliovirus outbreak was detected in the Philippines in 2019, and health workers are working to close a polio immunity gap present amongst some of the nation’s children. To successfully vaccinate children in Barangay 105 Happyland, the teams speak to community leaders, dodge traffic, and answer the questions of parents about the vaccine.
*This footage was recorded before the introduction of measures to reduce the spread of COVID-19 in the Philippines.
To find out more about the response, please visit WHO’s Polio Outbreak in the Philippines webpage
In March

In 2003, Melissa Corkum received a call that would change her life. The World Health Organization wanted to interview her for a position in their polio eradication team. Like most people who are hearing about polio eradication for the first time, the story compelled her, and she packed her bags to embark on a new adventure. Seventeen years later, she remains a dedicated champion of polio eradication.
A self-proclaimed ‘virus chaser’, Melissa has worked in all three polio endemic countries – Afghanistan, Pakistan and Nigeria. She found inspiration in her first field job in Nigeria, where she realized the scale of the polio eradication programme and that she was a part of something tremendous in public health history.
“I was amazed and inspired when I first saw the efforts of the front-line workers delivering vaccines to the doorstep. It may seem simple to deliver a couple drops into a child’s mouth, but when you see it in motion for the first time, it is truly remarkable,” Melissa said.

To this day, Melissa remains in awe of the work required to make ‘reaching every child’ possible. From mobilizing financial resources, to getting vaccines where they need to be while keeping them cool. From the microplanning to ensure all children and their houses are on a map, to the mobilization of champions in support of polio and immunization. Along the way, the stewards of these processes play an essential role to deliver the polio vaccine.
Melissa has worn many hats during her time in polio eradication, but her current role may be the most challenging yet. As the Polio Outbreak Response Senior Manager with UNICEF, she must answer the formidable challenge of containing outbreaks, using her expertise to inform global policy, strategy and operations.
To do this Melissa spent 80% of her time in the field prior to the outbreak of COVID-19, working with partners of the Global Polio Eradication Initiative (GPEI), Ministries of Health and local health workers.
Her work is a mix of challenge and excitement – the challenges of containing outbreaks, including those affected by the COVID-19 emergency – and excitement in developing new tools and methods to overcome the evolving challenges that present barriers to eradicating polio.
“There is never a dull day no matter what hat you may be wearing within this programme. If we are going to put an end to polio for good, we are going to have to fight the fight on a number of fronts – endemics and now the emerging issue of outbreaks in a post-COVID world,” said Melissa.
“The key is a willingness to do whatever it takes to get the job done.”
At times, Melissa felt the weight of the enormous challenges to eradicate polio, especially during her time in Afghanistan, where protracted conflict has complicated efforts to deliver basic services to the most vulnerable. Melissa often reflects on her time as Polio Team Lead there and the emotional rollercoaster she faced trying to stay ahead of the virus, while watching the tragedy of war unfold in the country.
“But when I felt down, I would pick myself up and get ready to face the next challenge. I found hope and inspiration in the resilience of the Afghan people, especially the women who worked in the polio programme, risking their lives and demonstrating a courage that stood out amidst all the difficulties.”

Melissa sees gender as one of the keys to polio eradication. She firmly believes that the only way to tighten the gaps in the system is by involving and empowering women equally in all roles across the programme, and that the only way to reach every child is to ensure their caregivers are equally informed and engaged in the decision making process.
“Unless we involve more women in the programme in certain corners of the world, we will continue to reach the same children and miss the same children, making polio eradication ever more difficult,” Melissa said.
“Change won’t happen if we don’t change the way we think about involving women. We need to listen to their views and open the doors for more women to join and participate equally from the community level and all the way to the leadership, decision-making level.”
Melissa was born in a small town in Nova Scotia, Canada. Her views on the critical involvement of women and gender equality in the polio programme very much align with her government’s Feminist Aid Policy. The Government of Canada has been a long-time champion of polio eradication and recently generously pledged C$ 190 million to assist the GPEI achieve its objectives of polio eradication.
Greater gender equity is one of the legacies that the polio programme is working to leave behind after eradication. Reflecting on her career, Melissa explains what keeps her working to defeat polio after all these years.
“It is so inspiring to be part of something tangible and something that is completely possible if we commit ourselves to doing everything possible to find every last child”.

In the midst of the COVID-19 pandemic, it is more critical than ever to recognize the power and importance of vaccines, which save millions of lives each year. Canada, the first government to contribute to the global effort to eradicate polio in 1986, has announced new investments to support immunization. Alongside renewed funding for Gavi, the Vaccine Alliance, the Honourable Karina Gould, Canada’s Minister of International Development, committed C$ 47.5 million annually over four years to support the Global Polio Eradication Initiative’s Endgame Strategy.
Due to widespread polio vaccination efforts over the past 30 years, more than 18 million people are walking today who would otherwise have been paralyzed, and cases have dropped by 99.9% thanks to the tireless efforts of health workers, local governments and global partners. The GPEI is proud to count on generous donors, including Canada, who have helped make this progress possible. This new investment will help the programme ensure gains made to date are not lost, resume activities as soon as it is feasible, implement strategies to overcome the remaining barriers to eradication, and further the dream of a polio-free world.
Minister Gould stated: “As a global community, we must work to ensure that those most vulnerable, including women and children, have access to vaccinations to keep them healthy wherever they live. COVID-19 has demonstrated that viruses do not know borders. Our health here in Canada depends on the health of everyone, everywhere. Together, we must build a more resilient planet.” The Minister added “The world has never been closer to eradicating polio, but the job is not done. With continued transmission in Afghanistan and Pakistan, we cannot afford to be complacent.”
Frontline polio workers in countries around the world are currently supporting the COVID-19 response, using networks established by the GPEI to focus on case detection, tracing, testing and data management. The G7 and the G20, including the Canadian Government, have recognized the important role GPEI assets play in strengthening health systems and advancing global health security, especially among the most vulnerable populations of the world.
In line with its feminist international assistance policy, Canada has encouraged the GPEI to build on the important role played by women in the programme, from the front lines to programme management and political leadership.
Akhil Iyer, Director of the Polio Eradication Programme at UNICEF said, “The new funding from the Canadian government is a testament to the major role played by the Canadian people in the historical fight against polio, and I am proud to be part of this endeavour as a Canadian citizen myself. Back in the 1950’s in Canada, poliovirus outbreaks could have paralysed or killed so many more children, and could have plagued the economy and pushed millions in vicious circles of poverty and ill health. But thanks to the scientific breakthrough of Dr. Leone Farrell who made mass production of polio vaccines possible, strong leadership and a learning health system, Canada was able to overcome the polio outbreaks and thrive during the following decades. It is more inspiring than ever, as we strive together to end polio from the world for good.”
Rotary clubs throughout Canada welcomed the new pledge as a continuation of the country’s leadership and partnership to end polio. Canada has worked closely with Rotary clubs in Canada since 1986 when Canada became a donor to GPEI. To date, Canadian Rotarians have raised and contributed more than US$ 41.3 million to eradication efforts.
Michel Zaffran, Director of the Polio Eradication Programme at the World Health Organization said, “I would like to express the profound gratitude of the GPEI partners to the Government and to the citizens of Canada for their tremendous support and engagement to end polio globally. The pandemic we are facing today is a stark reminder of the critical need for solidarity at all levels, international cooperation and of the power of vaccines and immunization. Canada is walking the talk: it is demonstrating once more its exemplary commitment to ensuring access to essential vaccinations, leading efforts to advance gender equality and reducing the burden of infectious diseases.”
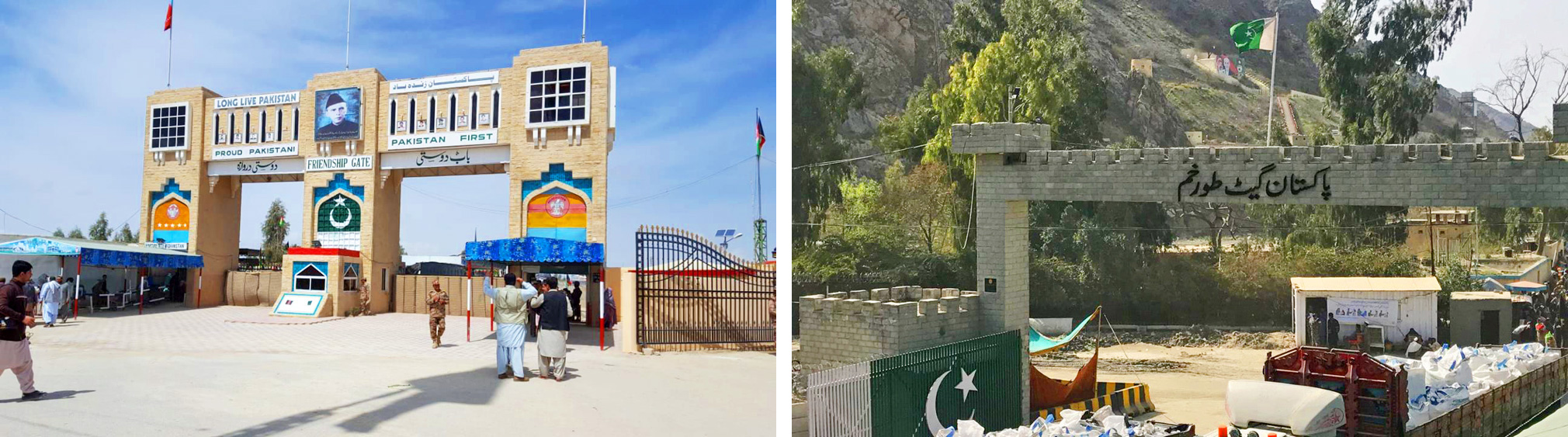
On both sides of the historical 2640-kilometre-long border between Pakistan and Afghanistan, communities maintain close familial ties with each other. The constant year-round cross border movement makes for easy wild poliovirus transmission in the common epidemiological block.

As a new tactic in their joint efforts to defeat poliovirus circulation, Afghanistan and Pakistan have introduced all-age polio vaccination for travellers crossing the international borders in efforts to increase general population immunity against polio and to help stop the cross-border transmission of poliovirus. The official inauguration of the all-age vaccination effort took place on 25 March 2019 at the border crossings in Friendship Gate (Chaman-Spin Boldak) in the south, and in Torkham in the north.
Although polio mainly affects children under the age of five, it can also paralyze older children and adults, especially in settings where most people are not well-immunized. Adults may play a role in poliovirus transmission, so ensuring that they have sufficient immunity is critical to simultaneously eliminating poliovirus from the highest risk areas on both sides of the Pakistan-Afghanistan border.
This is particularly important at the two main border crossing points – Friendship Gate and Torkham – given the extensive amount of daily movement. It is estimated that the Friendship Gate border alone receives a daily foot traffic of 30 000. Travellers include women and men of all ages, from children to the elderly.
Pakistan and Afghanistan first increased the age for polio vaccination at the border in January 2016, from children under five years to those up to 10 years old. The decision was in line with the recommendations of the Emergency Committee under the International Health Regulations (IHR) which declared the global spread of polio a “public health emergency of international concern”,
The all-age vaccination against polio at the border crossings serves a practical implementation of another recommendation of the IHR Committee: that Pakistan and Afghanistan should “further intensify crossborder efforts by significantly improving coordination at the national, regional and local levels to substantially increase vaccination coverage of travelers crossing the border and of high risk crossborder populations.”

As part of the newly introduced all-age vaccination, all people above 10 years of age who are given OPV at the border are issued a special card as proof of vaccination. The card remains valid for one year and exempts regular crossers from receiving the vaccination again. Children under 10 years of age will be vaccinated each time they cross the border.
Before all-age vaccination began at Friendship Gate and Torkham, public officials held extensive communication outreach both sides of the border to publicize the expansion of vaccination activities from children under 10 to all ages. Radio messages were played in regional languages, and community engagement sessions sensitized people who regularly travel across the border. Banners and posters were displayed at prominent locations.
Deputy Commissioner for Khyber District in Khyber Pakhtunkhwa province, Mr Mehmood Aslam Wazir, inaugurated the launch of All-Age Vaccination by vaccinating elderly persons at the Torkham border crossing. “Vaccination builds immunity and it is necessary for children to be vaccinated in every anti-polio campaign. The polio virus is in circulation and could be a threat to any child. The elders in our community could be carrier of the virus and take along the virus from one place to another, therefore, vaccination of every traveller, of all ages and genders, crossing Pakistan-Afghanistan border will be the key determinant to interrupt polio virus transmission in the region, and the world.”
The introduction of the all-age vaccination at border crossings is the latest example of cross-border cooperation between Pakistan and Afghanistan. The two countries continue to work closely together to ensure synchronization of strategies, tools and activities on both sides of the border.

In the wake of a polio outbreak confirmed on June 26 2018, the Government of Papua New Guinea declared polio a national health emergency. It was imperative that all children under the age of five be vaccinated, even those living in the most inaccessible regions of the country.
As part of the outbreak response, a team from Madang Provincial Health Authority, supported by WHO, travelled for over half a day by road and helicopter to reach the Hagahai people who live in the highlands of Madang province in Papua New Guinea, which is one of the most geographically isolated places in the world.
Ever wondered what it is like to be on the forefront of the fight against polio? Watch and learn how the team made their way to the remote mountain top to deliver vaccines.

In November, polio vaccination teams across Afghanistan targeted 5.3 million children under the age of five in high-risk provinces. The vaccination campaign came on the heels of several newly reported cases. Afghanistan has 19 documented cases of wild poliovirus in 2018, as of November. Confirmation of even one polio case anywhere signals remaining vaccination coverage gaps which must be filled to achieve eradication.
The targeted vaccination campaign took place from 5-9 November, and with support across the board from healthcare workers, communities, religious clerics, and the government. “The Ministry of Public Health and health partners are committed to ending this disease,” said Dr. Ferozuddin Feroz, Minister of Public Health.
Afghanistan is one of the three remaining endemic countries in the world along with Pakistan and Nigeria. The endemic countries are intensifying their efforts by making sure they fully implement the strategies in their national polio emergency action plans.
Read more about the details of Afghanistan’s vaccination campaign here.

Children clutch parents as the crowds gather. Overhead, clouds fill the sky, whilst below, noise rolls around the square where people stand. Shouts, music, and laughs all contribute to a growing sense of occasion.
The excitement lies at the heart of Karachi, Pakistan’s largest metropolis. Mazar-e-Quaid, the mausoleum of Pakistan’s founding father Muhammad Ali Jinnah, is a prominent symbol of Pakistani independence, and of the united people of Pakistan.
Each year, millions of people from across Pakistan and the world visit Mazar-e-Quaid. The number of visitors reaches its peak on 14 August, Pakistan’s Independence Day. As the sun rises, thousands arrive dressed in green, the national colour, carrying food and flags, ready to be first to enter once the site is opened up to the public.

For the Pakistan polio eradication programme, Independence Day is an important opportunity. From morning to night, they will take part in a herculean effort to vaccinate all children visiting the mausoleum against the poliovirus. In doing so, they are setting world records for the number of children vaccinated in one location.
Permanent Transit Points (PTPs) are vaccination sites established at important transit points such as country and district borders, bus terminals and railway stations, to make sure that children on the move are vaccinated against polio. Currently, there are 390 PTPs across Pakistan.
On an ordinary day, eight vaccinators work at a PTP at Mazar-e-Quaid. After a quick brief, they are ready to protect all visiting children from the virus with just two drops of the safe, effective oral polio vaccine.
Independence Day requires a different kind of operation. The teams know that they have to take the opportunity to vaccine young children who otherwise might miss out.
Twenty vaccinators volunteer, enthusiastic to meet the influx of parents with young children entering the site.
As the crowds surge into the mausoleum, vaccinators immunize a new child every few seconds at fixed points at the entrance and exit, whilst others mingle with the crowds, searching for any young child without a purple stained finger – the sign used to indicate that they have been vaccinated.
This year, 11 409 children were vaccinated at Mazar-e-Quaid over the course of Independence Day. With such a small team, this is an impressive achievement.

Mehwish Sheikh is a vaccination supervisor at Mazar-e-Quaid and is considered to be one of the most dynamic polio eradicators to have ever worked there.
Talking about her passion for polio eradication, and what drives her to protect Pakistan’s children, she says,
“Working against polio is in my blood. My mother started as polio worker in 1992 with the start of the polio eradication drive. Following her, I have worked for more than a decade now.”
“My mother vaccinated the current Chairman of Pakistan People’s Party Mr. Bilawal Bhutto Zardari, and she was featured on television and newspapers. My sister is also a vaccination worker so vaccination and work against polio is our passion.”
“Will you believe that I took only 3 days off on my wedding and then rejoined the team here?”, she laughs.
So what is it like vaccinating on Independence Day?
Mehwish isn’t afraid to acknowledge the challenges that the teams face on 14 August each year.
“This is really a tough day for all of us because the number of people is so overwhelming. Peoples’ connection with their leader is especially strong on Independence Day.”
With a wry smile, she continues, “Of course, our real independence will be our independence from polio virus.”
Whilst vaccination in this context might seem unexpected, parents visiting the Mausolem are enthusiastic. This is thanks to the efforts of the Pakistan polio programme and the government to educate the population about the vaccine.
One father notes, “As parents, it’s our duty to protect our children from going into harm’s way and administering all sorts of vaccines is one way of doing this.”
A nearby mother concurs, “The vaccinators are here to save the lives of our children and we must cooperate with them.”
The eradication of polio in Pakistan will be a success for thousands of people involved in the programme, and a source of national pride.
Speeding past to vaccinate more children, one vaccinator calls out, “We want to see our names among those who are fighting the final battle against polio in Pakistan”.
In April 2016, the polio programme embarked on a massive, coordinated effort to withdraw Sabin type-2 from routine use, through a synchronized switch from the trivalent formulation of the oral poliovirus vaccine (tOPV) to the bivalent form (bOPV). Over a two-week period, 155 countries and territories successfully made this change, marking the largest and fastest vaccine rollout in history.
Referred to as simply “the switch,” this global undertaking was a major programmatic achievement, but it was also a necessary step on the road to eradication. That’s because, in rare cases, the live, weakened virus contained in OPV can mutate and spread, resulting in cases of circulating vaccine-derived polioviruses (cVDPVs). The vast majority of these cases are caused by just one of the three components contained in tOPV (Sabin type-2 virus), so switching to a bivalent form that doesn’t contain this component was an attempt to significantly minimize the risk of further cVDPV2 cases – a decision that was endorsed by the global health community. Further, with Sabin type-2 responsible for 40% of vaccine-associated paralytic polio (VAPP) occurrences – a much rarer phenomenon at 2-4 cases per 1 million ‒ there was even stronger justification for the switch.
To assess whether the switch was successful, a group of researchers from Imperial College London, the World Health Organization and the Bill & Melinda Gates Foundation analysed stool and sewage samples from 112 countries collected in the first 15 months after the switch. The results, published in The New England Journal of Medicine, show that VDPVs and Sabin type-2 excreted into the environment after vaccination disappeared rapidly after the switch, shrinking to a much smaller geographic area.
These findings validate the GPEI decision to withdraw tOPV and demonstrate that the switch achieved its desired goal of reducing VDPVs and VAPP. This research also provides important evidence that the complete withdrawal of OPV after eradication of all wild polioviruses will eventually eliminate the risk of VDPVs, provided high immunity and effective surveillance are maintained. Eradication is simply not compatible with continued use of OPV.
The study also showed, however, that while some outbreaks of VDPV were expected post-switch, the number and magnitude of some of these outbreaks in different geographies has proven more difficult to control than expected. Type-2 VDPV outbreaks outside of Africa have been responded to with monovalent type-2 OPV (mOPV2) and controlled. However, outbreaks in the Horn of Africa, DR Congo and Nigeria have been very difficult to bring to a rapid close.
VDPV outbreaks emerge in areas with very low population immunity, due to low immunization coverage. Factors which enable them ‒ insecurity and resulting inaccessibility, weak health systems, and poor campaign performance – are the same that need to be addressed to stop their transmission. While the programme is aware of these risk factors and has proven experience and strategies to respond to them, the longer outbreaks persist, the harder they can be to stop.
The key to stopping these outbreaks will be to increase the focus on improving the quality of vaccination campaigns in accessible areas. In inaccessible areas, we need to use all available means to negotiate access and implement vaccination campaigns. Achieving high quality campaign activities will give us the best chance to stop all types of poliovirus for good and prevent any child from being paralysed by the virus ever again.
Reposted with permission from gavi.org.

This is southern Afghanistan. A place characterized by a rich, diverse, but often complex history. Enveloped by mountains, this part of the country has seen years of conflict which have left hospitals under-resourced and health services shattered. Children face many challenges – as well as conflict and poverty, southern Afghanistan has the highest number of polio cases in the world.
In this difficult environment, the virus can only be defeated if every child is vaccinated.

Afia (not her real name), who is nineteen years old, is one of over 70 000 committed polio workers in Afghanistan, supported by WHO and UNICEF. Last month, she and her colleagues vaccinated 9.9 million children and educated thousands of parents about vaccination across the country.
The polio eradication programme comprises one of the biggest female workforces in Afghanistan: a national team, all fighting polio. Some women work as vaccinators, whilst others, like Afia, are mostly engaged in education and social mobilisation efforts. The polio programme gives women culturally-appropriate opportunities to work outside the house and engage in their community, speaking to parents about the safe, effective polio vaccine, and answering their questions. Often, women vaccinators offer other kinds of health advice, including recommendations for good child and maternal health.
To be a good vaccinator and educator, women must be committed to better health for all, with strong communication skills. They must also be organized to ensure that every child is reached during the campaign.
Afia says that if she wasn’t eradicating polio, her parents would expect her to give up her education and get married. Her younger sisters look up to her, excited to work in the polio eradication programme when they are old enough.
Her job is very important to protect all children. Afghanistan is just one of three countries – the others are Nigeria and Pakistan - that have never interrupted poliovirus transmission.
Women can vaccinate children who might otherwise miss out. Culturally, male vaccinators are unable to enter households to administer vaccine, causing difficulties if young children are asleep or playing inside. Their freedom to enter homes and give the vaccine to every child is one reason female polio workers are so critical.
Afia started work at 7 am, and is now walking home ten hours later with a young boy she has just vaccinated. Her purple burka stands out against the sand as she goes home to tell her parents and siblings about her day.
Afia feels positive about the future of polio eradication in Afghanistan: “We have a duty to protect our children, and I won’t stop working until every child is protected.”
Women have a right to participate in all aspects of polio eradication. Removing barriers to women’s full participation at all levels is a key goal for the Global Polio Eradication Initiative (GPEI). To learn more, see the gender section of our website, and read the GPEI ‘Why Women’ Infographic.


Molvi Hameedullah Hameedi is a prominent religious scholar in a mountainous rural area of Killa Abdullah district, one of the poorest districts in Balochistan province, Pakistan. With a close connection to his community, who are mostly Pashtuns, he delivers the sermon each week during Friday prayers, and runs a religious seminary.
He is also a determined supporter of routine vaccination for all children, and an advocate for better health.
This might come as a surprise if you met Molvi Hameedullah just a year or two ago. For most of his life, he did not believe in the safety and effectiveness of the oral polio vaccine, the key tool of polio eradication.
“I was a religious scholar who was very sceptical of non-governmental organizations and the polio vaccine,” he reflects.
“After reading anti-vaccine books and papers, I began following the work of anti-vaccine campaigners. Soon, I came to consider it my religious duty to spread awareness against the polio vaccine.”
“But it all changed when I was invited to a two-day International Ulema conference in Islamabad where religious scholars from all over Pakistan and other Islamic countries were invited to debate polio vaccination.”
The conference Molvi Hameedullah attended was hosted by the Islamic Advisory Group for Polio Eradication (IAG). The IAG was launched in 2014 by leading Islamic institutions including Al-Azhar University, the International Islamic Fiqh Academy (IIFA), the Islamic Development Bank (IsDB) and the Organization of Islamic Cooperation (OIC).
For Molvi Hameedullah, attending the conference marked the beginning of a change in perspective. “At the conference, I was given an opportunity to discuss my apprehensions towards polio vaccine. The talks I had motivated me to further research the pro-polio vaccine stance, and I started meeting with religious scholars in Karachi to debate polio vaccination.”
“Through talking to these people, I was getting a completely different picture to what I had believed earlier.”
By educating religious leaders and scholars about the poliovirus, and explaining religious justifications for vaccine acceptance, the IAG and its national equivalent equip people like Molvi Hameedullah with the tools to act as health advocates. The same skills that help scholars engage with parents about the polio vaccine are applicable for wider health, including improving routine immunization, hygiene practices, and maternal and child health.
After the conference Molvi Hameedullah was offered support by other vaccine-promoting scholars.
“I received a book from a religious support person working for polio vaccination in my area. Included were dozens of fatwas from highly esteemed madrassahs and religious teachers. I was initially sceptical, so I telephoned the madrassahs who had written them. To my surprise, all the fatwas were genuinely issued by them, and they also urged me to support vaccination wherever I called.”
Today, Molvi Hameedullah teaches similar fatwas as a member of the Provincial Scholar Task Force under the National Islamic Advisory Group. Most Task Force members have an honorary position, and are not paid a salary. Instead, the local government facilitates their transport and communication needs during immunization campaigns. Of his new role Molvi Hameedullah says, “I was faced with a different problem. I had been working against polio vaccination for many years, and now felt that I had done a great damage to the children and parents of my community. I felt it was now my absolute religious duty to negate all that I had taught before. I decided to step forth, and started working in the community voluntarily to promote vaccination.”
Religious refusals in Molvi Hameedullah’s area have declined. He has begun supporting other ways of ensuring that every child receives a vaccine, including by recruiting women vaccinators.
He acknowledges that the work he does now is not easy. He and his fellow scholars sometimes face challenges from those accusing them of having a political agenda, and changing beliefs informed by years of cultural and religious tradition takes time and patience. But he vows to continue his new mission until eradication.
There have been no cases of polio in the area of the district that Molvi Hameedullah covers since he joined the Provincial Scholars Task Force. Looking ahead, he is determined not to stop until all of Pakistan is polio-free.
