Surveillance is at the heart of the drive to protect children against polio. Click through these pictures to learn about the journey from child to laboratory, the people behind the process and the ways in which polio surveillance in Bangladesh is contributing to surveillance for other diseases.
In cities and villages all over Bangladesh, networks of teachers, religious and local leaders, students, and doctors like Luna Unnekamrun are alert for signs of Acute Flaccid Paralysis (AFP), the symptoms that give a warning that polio might be circulating in the area. Whenever a child is recognised as having the symptoms of AFP, they are taken to a sub-district level hospital, where a Government Medical Officer or Surveillance Medical Officer (SMO) from WHO meets them to take a sample for testing.
'The role of a Surveillance Medical Officer nowadays is to prove the absence of polio, which is just as important as actually finding it.’ Explains Dr Tanbirul Islam, WHO. ‘To eradicate a disease like polio, you have to be able to find the virus. But you can’t see it with the naked eye, so we look for the symptoms. If we get samples as soon as possible and prove whether or not it is polio, we can find out what to do next.'
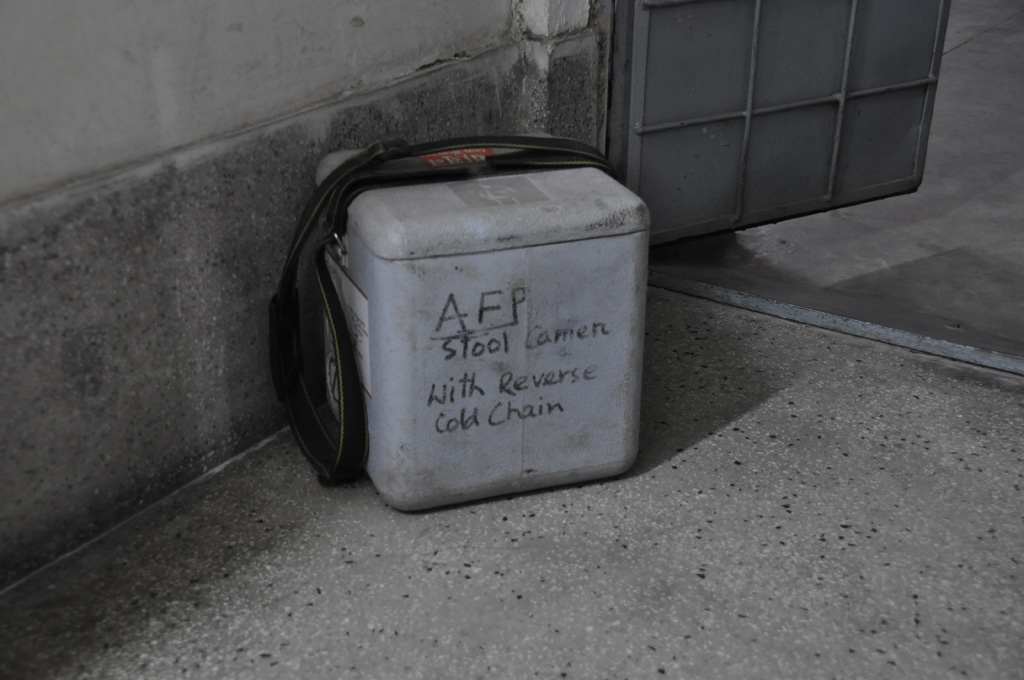
Two stool samples from every child with AFP, taken hours apart, are carefully packaged and stored by the SMO ready to be transported to the National Polio and Measles Laboratory in Dhaka. Each sample must travel with four ice packs, and must reach the laboratory within 12 hours of having left the hospital, even when travelling from the furthermost districts of Bangladesh.
Dr Mahbuba Jamil is a virologist and the Manager of the National Polio and Measles Laboratory in Bangladesh. Established in 1953, it has been operational for over 60 years, and has been the national hub for polio surveillance 1997. Here, some of the most important work to tackle polio in Bangladesh takes place.
In the sample receiving room, each delivery is recorded. In 2014, 3112 samples were received and processed at this laboratory from all over Bangladesh. From here, they are taken into the sample processing room. In isolation, the sample is opened and processed. Per child, 4 are tested for the virus. This process can take 2 to 5 days.
From the processing room onwards, extensive biosecurity measures must be taken to ensure no virus that might be in the sample can spread. The technician must wear gloves, lab coat and shoes, and no member of staff works across two stages of the process. Only those who work in each room have the key to the samples; even Dr Jamil as Laboratory Manager doesn’t have a copy. In the inoculation laboratory in the next room, 200 micro-litres of the cells are checked every day for 5 days. It can take up to ten days to test for the presence of polio at this stage. If a sample tests positive, it is mixed with reagents that confirm without a doubt whether the poliovirus is present in the sample.
Polio was eradicated in Bangladesh in 2000. But while the virus continues to circulate in nearby countries such as Pakistan, keeping surveillance strong is crucial to ensure the virus doesn’t return unnoticed. This year, Bangladesh will begin to test for polioviruses in the environment. Sites have been selected where the sewage system is exposed, like in waterways. Every month, a sample from these sites will be tested for the virus. This is a very ambitious project for such a small laboratory to take on, but it is crucial to make sure they are aware of the virus in the shortest possible period of time, enabling the response to be rapid and effective.
While AFP surveillance remains as important as ever, the eradication of polio in Bangladesh has enabled staff from the laboratory to begin working on surveillance for other diseases. The expertise built up by the polio staff here is extensive. Six staff members now work full time testing blood samples for measles. As we move towards the global eradication of polio, the number of diseases that will be able to benefit from the expertise in this laboratory will grow. This is an example of the legacy that polio staff, infrastructure such as laboratories and lessons learned can leave beyond polio.
Results from every single sample that passes through the laboratory is fed into the data system by staff like Mr Sharifuzzaman, who can tell you details of cases stretching back to 1997. This data is then analysed and used for planning and decision making. This full cycle from each case of AFP to laboratory to planning is well oiled in Bangladesh. “This began in the polio eradication culture, and then expanded out into EPI in general. Polio had the resources to go right down to the micro level. And because many of those currently in the workforce were also here in those early days, the skills have been able to spread,” says Dr N. Paranietharan, Head of Country Office in Bangladesh.
The plans that are produced at the end of this process enable the Expanded Program on Immunization and WHO to be sure that no children remain vulnerable to poliovirus. Being sure that the virus is gone for good is as important as knowing when it is there. The polio surveillance cycle begins with a child whose life has been devastated by paralysis, but will end with generations of children free from the threat of polio.