News Category: Broader benefits of the polio programme

In London on 19-20 April, leaders of the 53 member states of the Commonwealth affirmed their commitment to end polio in the final Communique of the 2018 meeting. Leaders emphasized renewed support for international efforts to tackle polio and other diseases, and called for an increase in national health expenditure throughout the Commonwealth.
This outcome was largely thanks to the efforts of civil society, including outreach by members of Rotary clubs in Commonwealth countries, Global Citizen, and numerous other partners who urged Commonwealth leaders to uphold their commitment to polio eradication. This included the delivery of over 4000 messages to UK Prime Minister Theresa May appealing for her continued commitment to a polio free world.
Throughout the course of the summit and related events, individual leaders also voiced their continued support for eradication. Prince Charles, who will one day succeed Queen Elizabeth II as Head of the Commonwealth, held up the polio programme as an example of successful joint action against disease and noted that hundreds of millions of children have benefitted from polio vaccine because of the GPEI. The end of polio, he noted, will serve as an example of the Commonwealth’s proven track record in effecting change. Once eradication is achieved, polio infrastructure will be leveraged to address other health challenges, and may pave the way for malaria elimination. Incoming Chair of the Commonwealth Theresa May, in a direct letter to advocates, acknowledged that eradication “remains a top global priority,” and promised that the UK will “work closely with polio-endemic countries to ensure we eradicate this cruel disease, once and for all.” Malta’s Prime Minister Joseph Muscat, who has championed polio throughout his tenure as Commonwealth Chair, pledged during a speech to help end polio in Commonwealth countries Pakistan and Nigeria.
With a collective investment of more than US$ 4 billion and previous statements of commitment to polio eradication, Commonwealth governments have long-been leading champions to end polio. As Bill Gates noted during his summit remarks, “success [against polio] really goes back to the substantial commitments made in part at the Commonwealth meetings.” With a record low 22 cases registered last year, continued global support is vital to get the world over the finish line. The renewed support from the Commonwealth, which represents a wide range of countries, provides hope that governments remain firmly committed to fulfilling the promise of a polio-free world.

Fear of paralysis, severe illness, or death from polio and smallpox was a very real and pervasive reality for people worldwide within living memory.
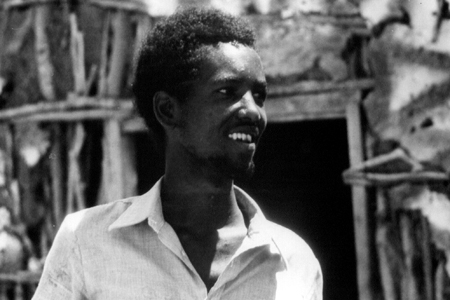
In 1977, the world was close to finally being smallpox free. The number of people infected had dwindled to only one man; a young hospital cook and health worker from Merca, Somalia named Ali Maaow Malin.
Before Ali, smallpox had affected the human population for three millennia, infecting the young, the old, the rich, the poor, the weak and the resilient.
Spread by a cough or sneeze, smallpox caused deadly rashes, lesions, high fevers and painful headaches – and killed up to 30% of its victims, while leaving some of its survivors blind or disfigured.
An estimated 300 million people died from smallpox in the 20th century alone, and more than half a million died every year before the launch of the global eradication programme.
The power of a vaccine
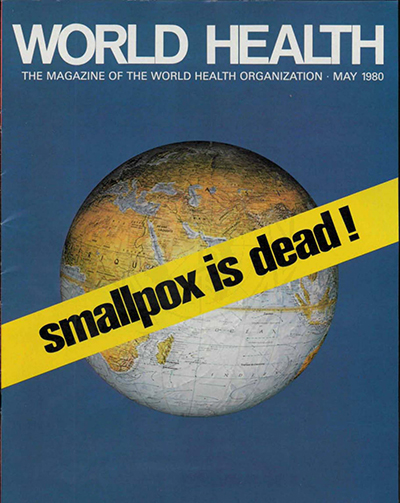
Between 1967 and 1980, intensified global efforts to protect every child reduced cases of smallpox and increased global population immunity. Following Ali’s infection, the World Health Organization carefully monitored him and his contacts for two years, whilst maintaining high community vaccination rates to ensure that no more infection occurred.
Three years later, smallpox was officially declared the first disease to be eradicated. This was a breakthrough unlike any other – the first time humans had definitively beaten a disease.
But smallpox wasn’t the only deadly virus around
On March 26, 1953, Dr Jonas Salk announced that he had developed the first effective vaccine against polio. This news rippled quickly across the globe, leaving millions optimistic for an end to the debilitating virus.
Polio, like smallpox, was feared by communities worldwide. The virus attacks the nervous system and causes varying degrees of paralysis, and sometimes even death. Treatments were limited to painful physiotherapy or contraptions like the “iron lung,” which helped patients breathe if their lungs were affected.
Thanks to a safe, effective vaccine, children were finally able to gain protection from infection. In 1961, Albert Sabin pioneered the more easily administered oral polio vaccine, and in 1988, the Global Polio Eradication Initiative was launched, with the aim of reaching every child worldwide with polio vaccines. Today, more than 17 million people are walking, who would otherwise have been paralyzed. There remain only three countries – Afghanistan, Pakistan, and Nigeria – where the poliovirus continues to paralyze children. We are close to full eradication of the virus – in Pakistan cases have dropped from 35 000 each year to only eight in 2017.
Since there is no cure for polio, the infection can only be prevented through vaccinations. The polio vaccine, given multiple times, protects a child for life.
Better health for all
Thanks to vaccines, the broader global disease burden has dropped drastically, with an estimated 2.5 million lives saved every year from diphtheria, tetanus, pertussis (whooping cough), and measles. This has contributed to a reduction in child mortality by more than half since 1990. Thanks to an integrated approach to health, multiple childhood illnesses have also been prevented through the systematic administration of vitamin A drops during polio immunization activities.
Moreover, good health permeates into societies, communities, countries and beyond – some research suggesting that every dollar spent vaccinating yields an estimated US$ 44 in economic returns, by ensuring children grow up healthy and are able to reach their full potential.
Ali Maaow Malin, the last known man with smallpox, eventually made a full recovery. A lifelong advocate for vaccination, Ali went on to support polio eradication efforts – using vaccines to support better health for countless people.
Without the life changing impact of vaccines, our world would be a very different place indeed.

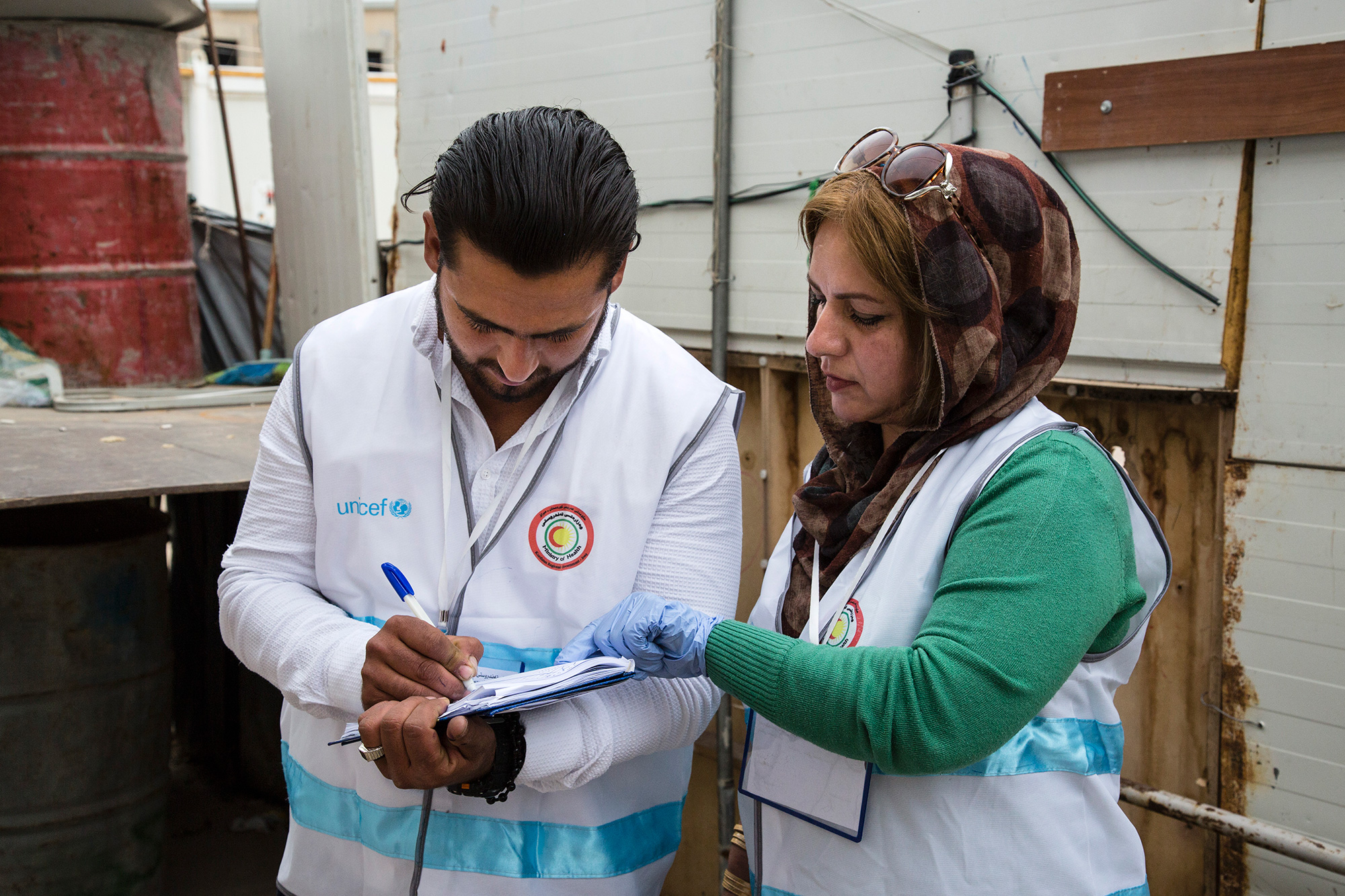
Efforts to protect children from polio take place all over the world, in cities, in villages, at border checkpoints, and amongst some of the most difficult-to-access communities on earth. Vaccinators make it their job to immunize every child, everywhere.
In places where families are displaced and on the move due to conflict, it is especially important to ensure high population immunity, to protect all children and to prevent virus spread. In Iraq last month, vaccinators undertook a five-day campaign in five camps for internally displaced people around Erbil, in the north of the country, as part of the first spring Subnational Polio campaign targeting 1.6 million children in the high risk areas of Iraq (mainly in internally displaced person camps, and newly accessible areas).

Binta Tijjani works to eradicate polio in her native Kano state of Nigeria. She is one of the over 360 000 frontline workers dedicated to ending polio in her country, the vast majority of whom are women. Nigeria is one of only three countries in the world yet to stop poliovirus circulation, together with Afghanistan and Pakistan.
Binta has worked in polio eradication for over 14 years. Starting as a house-to-house vaccination recorder, she was soon promoted to the role of polio campaign supervisor and now works as an independent polio campaign monitor.
“My biggest strength is my ability to work closely with our teams to ensure we reach every last child with vaccines, and advising teams so they can ask the right questions and raise important issues in each household they visit,” Binta says.
Working with the polio programme often opens up other opportunities for women to enter the workforce and utilize their skills to contribute to their communities, leading to positive investments beyond polio eradication.
“My work with the polio programme has enabled me to buy land and take care of my children’s school fees and our household needs. Currently I’ve enrolled in a course to get a certificate in catering. My dream is one day to open a restaurant,” Binta says.

Similar to Binta, Halima Waziri has been serving the polio eradication cause in different roles since 2005. Currently Halima works as a lot quality assurance sampling interpreter in Kano state, assessing the quality of vaccination coverage after immunization campaigns in her area.
“I am most proud of engaging in many productive dialogues about polio vaccination in remote and hard-to-reach areas and high-risk communities in Nigeria. This has helped me to improve my interpersonal communication skills and given me confidence in public speaking and influencing people,” Halima says.
With the money she has earned as a polio worker, Halima has opened a medicine store where she sells medicines and also acts as a community informant and focal point for disease surveillance.
Nigeria was on the brink of eradicating polio when a new wild poliovirus case was reported in 2016 after two years without any confirmed cases. Low overall routine immunization coverage is a key stumbling block to eradication, combined with ongoing violent conflict in the northeast where over 100 000 children remain inaccessible for vaccination teams.
Nigeria continues to implement an emergency response to vaccinate all children under the age of 5 to ensure they are immunized and protected, including implementing vaccination campaigns whenever security permits, vaccinating children at markets and cross-border points, and conducting active outreach to internally displaced people.
Without the critical participation of women as vaccinators, surveillance officers and social mobilizers, Nigeria would not be as close to eradicating polio as it is today. The latest nationwide immunization campaign, synchronized with countries in the Lake Chad basin, aimed to reach over 30 million children in Nigeria in April.
No wild poliovirus cases have been reported in 2017 or 2018. Binta and Halima, together with an army of frontline workers, are determined to keep it this way and secure a polio-free future for Nigeria.

From the front passenger seat of a small utility truck, Mahmoud Al-Sabr hangs out the window, looking for families and any child under five years old to be vaccinated against polio. As the car he travels in dodges rubble and remnants of buildings that once stood tall in Raqqa city, he flicks the ‘on’ switch for his megaphone.
“From today up to January 20, free and safe vaccine, all children must be vaccinated to be protected from the poliovirus that hit Syria for the second time,” he calls, beckoning families with young children who have recently returned to Raqqa city to come outside of their makeshift homes amongst destroyed buildings, to have their children vaccinated.
In 2017, amidst the protracted conflict and humanitarian crisis in Syria, an outbreak of circulating vaccine-derived poliovirus type 2 (cVDPV2) was detected, threatening an already vulnerable population.
Due to ongoing conflict, Raqqa city, which was once host to half of the governorates population, had been unreached by any vaccination activity or health service since April 2016. During the first phase of the outbreak response, more than 350,000 resident, refugee and displaced children were vaccinated against polio in Syria, but “Raqqa city remained inaccessible,” says Mahmoud.
In January 2018, polio vaccinators conducted the first vaccination activity in the city since it became accessible again, following the end of armed opposition group control.
There were no longer accurate maps or microplans that vaccinators could use to guide them in their work. Unrecognizable, the city was a picture of devastation with few dwellings untouched by the violence that once caused families to flee. The house-to-house vaccination campaign that usually helps the programme to reach every child under five wouldn’t work here. Teams knew they would have to innovate to seek out families wherever they were residing to vaccinate their children.
“All children must be vaccinated to protect against poliovirus,” Mahmoud echoes around shelled out buildings, and slowly mothers and fathers carrying their children start to appear in the street.
Mahmoud and Ahmed Al-Ibraim are one of 12 mobile teams that are going street by street, building by building, by car in search of children to vaccinate. Carrying megaphones to alert families of their presence and to tell them of the precious vaccines they carry that will protect their children from the paralysing but preventable poliovirus, they slowly cover areas of the city now unrecognizable.
“No one could enter Raqqa City now for two years,” says Abdul-Latif Al-Mousa, a lawyer from the city who joined the outbreak response as a Raqqa City supervisor for polio campaigns. “So children have not been vaccinated here since that time. Now that people have returned, we are learning where they have returned from and we vaccinate them regardless.”
“We must reach each child with the vaccine to protect them – polio is preventable, why should they suffer more?” Ahmed appeals.
Campaign brings vaccines and familiar faces
Vaccines were not the only thing to return to Raqqa City in January. It was the first time that WHO polio focal point Dr Almothanna could return to Raqqa City after being force to flee under the rule of the armed opposition group. Imprisoned for refusing the demands of the group, friends and neighbours of Dr Almothanna facilitated his escape from the city in 2016.
Dissatisfied but not deterred, Dr Almothanna continued to work with the polio programme, serving the whole governorate except his own city. Over the course of the January 2018 campaign, he worked tirelessly with vaccination teams to ensure more than 20 000 children under the age of five in Raqqa City received a dose of mOPV2 to protect them against polio. For many, it was the first vaccination they had received. In the additional campaigns that followed in March 2018, even more children were reached.
The microplans developed by vaccinator teams in the first vaccination round have become a critical road map for reaching children and families with health services, accounting for the locations of returned families and information about neighbouring families that teams had not yet located. In the second round, the microplans were updated to include new families who had returned.
Syria reported 74 circulating vaccine-derived poliovirus cases between March and September 2017. It has been more than six months since the last case was reported (21 September 2017). Efforts are continuing to boost immunity in vulnerable populations, maintain sensitive surveillance for polioviruses and strengthen routine immunization to enhance the population immunity.

“When I received the confirmation of the first case of Lassa fever…nothing prepared me for the tasks ahead other than my work in polio eradication” – Mrs Faith Ireye, WHO State Coordinator in Edo state.
In the first two months of 2018, there were 110 deaths in Nigeria from suspected Lassa fever. Outbreak response, led by the Nigerian government and WHO, is focused on detecting every case, and tracing the virus wherever it is hiding.
Bolstering this effort are individuals with experience of guarding against a different disease – polio.
Ms Ireye, who has worked with the Global Polio Eradication Initiative for over ten years, is currently helping to coordinate the Lassa fever outbreak response in Edo State, one of the hardest hit by the outbreak.
“My experiences in polio eradication activities allowed me to immediately swing into action. So, when the [Lassa fever] outbreak was confirmed, I realized the need to use my expertise to serve communities at risk,” she says.
Part of her job is to help coordinate surveillance, specifically ensuring that everyone who has come into contact with someone with Lassa fever is found, and tested for the virus.
Her work is critical to help prevent further fever cases. Deputy Governor of Edo State, His Excellency Philip Shaibu said, “WHO…is one of the pillars that have helped lead surveillance in Edo state… In this particular outbreak, WHO was the first to draw attention to the fact that we need to galvanize resources from all partners, from other parts of the country, to ensure that things get done.”
The polio infrastructure
When outbreaks of other diseases happen, the knowledge and experience of polio personnel like Ms Ireye can make a significant difference to outbreak response. For example, polio workers were essential to containing the Ebola virus outbreak in 2014. For the Lassa fever response, 271 polio workers are involved in active case search, 235 in contact tracing, and 320 in community sensitization activities across the 18 at-risk states.
“The polio infrastructure was originally designed towards achieving the polio eradication goals,” said Dr Wondimagegnehu Alemu, WHO Country Representative to Nigeria. “Now polio infrastructure has expanded its support to broader disease surveillance strengthening, outbreak response and basic health care services including immunization.”
The benefits of experienced personnel

Other activities carried out by polio workers include data collation and analysis, and case reporting.
“The polio teams on ground in the states were crucial for mounting the initial response to the Lassa fever outbreak, and have continued to be WHO’s frontline technical support to the NCDC, States Ministry of Health and local government area teams,” Dr Emmanuel Musa, WHO Incident Manager for Lassa fever Management Team in Nigeria observed.
A legacy for posterity
Investments by donors and partners have gone far beyond polio eradication. Reflecting the positive impact that polio infrastructure and knowledge has had on other health priorities such as Lassa fever, WHO and other partners are currently supporting the development of a national transition plan. This will ensure that the investments that have brought the world to the brink of eradication are made available to support other national public health efforts, long after polio has been defeated.
“We must carefully consider how we transition many of the polio workers and the polio infrastructure to help with managing other health needs,” Dr Alemu said. “Future funding and partnerships will be a key part of this work.”
For now, experienced polio personnel continue their work to end the Lassa fever outbreak. Thanks to them, and the support of governments, partners and donors, we are ending polio, and are also helping to strengthen other health interventions.
Support for immunization to the Federal Government of Nigeria through the World Health Organization is made possible by funding from the Bill & Melinda Gates Foundation (BMGF), the United Kingdom, the European Union (EU), Gavi, Global Affairs Canada (GAC), the Government of Germany, the Japan International Cooperation Agency (JICA), the Korea Foundation for International Healthcare (KOFIH), the Measles and Rubella Initiative (M&RI) through the United Nations Foundation (UNF), Rotary International, the United States Agency for International Development (USAID), the United States Centers for Disease Control and Prevention (CDC) and the World Bank.


Reducing polio cases by 99.9% globally is an incredible feat, achieved through innovative strategies and years of trial and error.
While the polio eradication programme is focused on getting to zero, now is the time to make sure everything we’ve learned isn’t lost and can be used to inform future global health programmes. Just as the polio eradication effort applied lessons learned from the successful smallpox campaign to its own work, the goal is for future health programmes to understand and build on the knowledge of the polio effort.
Under a new grant from the Bill & Melinda Gates Foundation, the Johns Hopkins Bloomberg School of Public Health (JHSPH) will be working to do exactly this.
JHSPH will partner with academic institutions from around the world to document lessons and develop graduate-level courses and hands-on training clinics for public health students and professionals, including an online open course available to the public and implementation courses for managers from other health programmes.
Under the leadership of Dr Olakunle Alonge, the team at JHSPH will collaborate with a global team from public health institutions in seven countries: Nigeria, India, Afghanistan, Ethiopia, the Democratic Republic of the Congo, Bangladesh and Indonesia. This will not only ensure a balanced and diverse perspective, but also enable the exchange of public health training strategies between the institutions.
To develop the content of each course, JHSPH will be identifying “change agents” at the local, national and global levels who have expertise in polio eradication that may not otherwise be captured. This unique global strategy promises to yield coursework that speaks to the issues faced by a broad range of global health programmes and actors.
“Without an active strategy to map, package and deliver the knowledge from the global polio eradication efforts to other programs and global health actors, I’m afraid that these knowledge assets may not find any useful purpose beyond the end of the polio campaign, which could come to an end within a few years,” said Alonge.
Alonge expects to glean lessons that will apply to immunization systems, public health emergency response, primary health care, disease eradication and infectious diseases—ensuring that the polio programme continues to positively impact global health for years to come.
“I feel our collective productivity has improved manifold, ever since we started working together with the Community Based Vaccinators from the polio eradication programme,” says Syed Mussayab Shah, a tone of pride in his voice. Shah is a vaccinator with the Expanded Programme of Immunization, posted at Gulbahar Civil Dispensary, Peshawar district, Khyber Pakhtunkhwa. He is responsible for immunizing children against nine vaccine-preventable childhood diseases.
Reaching children with vaccines in dense urban environments can be a significant challenge. So the polio eradication programme and the team responsible for delivering routine vaccines – the Expanded Programme on Immunization – are working together to make sure that they do the job as best they can, explains Shah. “We are determined to reach and vaccinate every child in our area. And to ensure this, we exchange information and notes with the community based vaccinators twice every week.”
| “The synergy between the two programmes has been a blessing as we are reaching more children with vaccination every day, including those living in urban slums. Our spirits are high and we are determined to reach every last child.” Dr Akram Shah |
Vaccination challenges in urban areas
Where families live in concrete housing units in urban slums, access to health care is a persistent challenge. The urban slums are often unrecognized, lack essential infrastructure and are low priority for local health authorities. This translates into low and unequitable coverage of social services in urban areas – including vaccination.
Pakistan is the most urbanized country in South Asia and the population living in urban slums continues to increase. The urban population has risen from an estimated 43 million in 1998 to 73 million in 2014. In Peshawar, increased migration is an additional challenge, making it the sixth biggest city in the country.
The challenge of identifying and vaccinating children living in urban areas, especially those living in slums and migrant families, is demanding innovation and skill sharing. The teamwork between the polio eradication team and the Expanded Programme for Immunization is ensuring everyone benefits – especially children who urgently need the protection offered by vaccines.
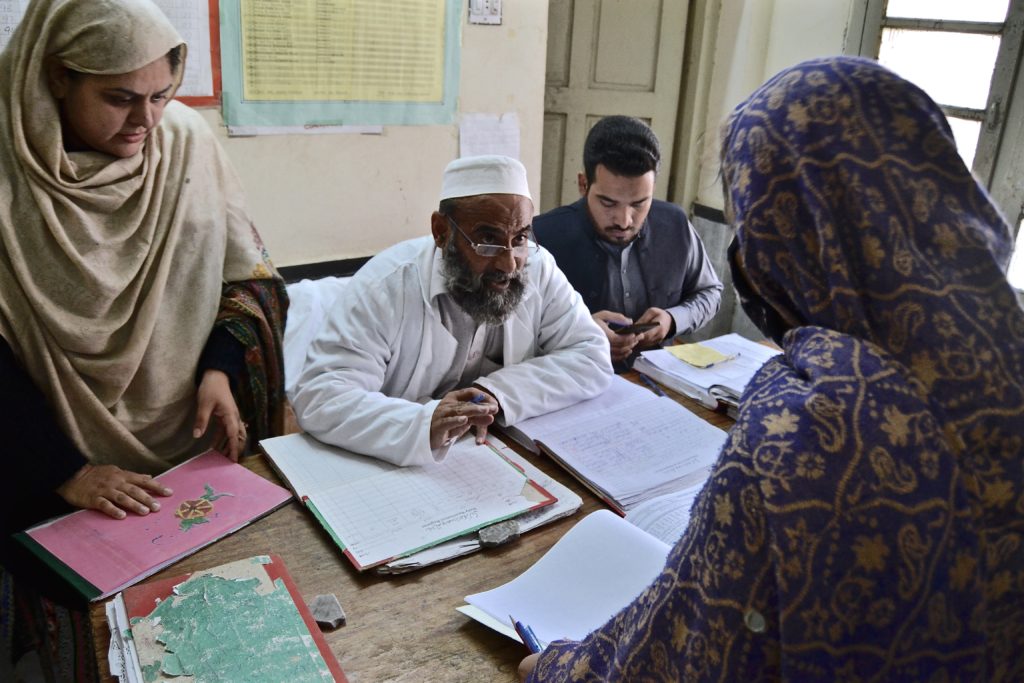
Increasing vaccination coverage through collaboration

The Civil Dispensary is the only government health facility in the area that caters not only to the residents of Gulbahar but also those living in adjoining slums. Community-based polio vaccinators from local areas come to this health facility to sit side by side with their colleagues from the broader vaccination programme to review their field books containing the housing maps and vaccination details of every single child under five in their areas. Microplans, containing this detailed information of local communities, are a valuable tool of the polio eradication programme. From this essential information, routine vaccinators make a list of unvaccinated children for follow-up who might be falling through the cracks. The polio vaccinators also refer clients from their communities to the health facility to receive their other routine vaccines. This collaboration is game changing for the drive to protect every last child against vaccine preventable disease.
UNICEF, with funding from Gavi, the Vaccine Alliance, is supporting the Government of Pakistan in improving routine immunization coverage in urban slums with a focus on seven major cities in Pakistan in collaboration with the polio eradication programme.Referring to the synergy initiative, Shah says, “Earlier we worked without defined plans and targets. Now, due to the information sharing from community based polio vaccinators, we have plans with identified areas and targets that help us monitor our own progress as well as the vaccination coverage.”
“Record keeping of families in urban slums is a very difficult job,” shares Tabassum Shuaib, a polio community-based vaccinator from Peera Gaib, Peshawar.
Teamwork paying off
“Families are constantly moving in and out from here – and many of those that move in do not have a vaccination card. They can only recall the number of times their child has been vaccinated. However, now I have all the families, pregnant mothers and children under five from this community registered and their data is maintained at the Gulbahar Civil Dispensary, so we can keep track ourselves and make sure no child is missed.”

Dr Akram Shah, Director of the Expanded Programme of Immunization in the area, is pleased with the rewards of this teamwork: “Peshawar offers the same challenges as any other major city of Pakistan. With increased migrant population and urbanization during the past decade, the burden of ensuring access to basic life and health resources to all has also increased. The synergy between the two programmes has been a blessing as we are reaching more children with vaccination every day, including those living in urban slums. Our spirits are high and we are determined to reach every last child.”

Outside a sandy coloured building in a village in Burkina Faso, a young girl on crutches is making her way out onto the street. In front of her home is a new wheelchair – child-sized, brightly painted and specially adapted to the unpaved streets of her neighbourhood.
Countries around the world are united in their efforts to eradicate polio so that it will never again cause a child to be paralysed. This is important because there is no cure to this paralysing disease. For polio survivors in Burkina Faso, the opportunity to be independently mobile in their own communities can be life changing.
Independence after disability
For children living in poor communities whose limbs are paralyzed by polio, there is often very little support available to make them independently mobile. Giving a child a wheelchair puts previously inaccessible opportunities within reach so that children can reach their potential; such as going to school, playing outside with friends and learning new skills. In many cases the children are free to explore the world around them for the first time without a friend or family member to help.
Rotary International, along with partners such as Sahel, are providing support to the AMPO Association in Ouagadougou to provide services and facilities for children, teenagers, young mothers and people with disabilities often caused by polio.
Custom-made wheelchairs
The tricycles are hand-crank operated by the individual to navigate the difficult roads of Burkina Faso. A wider version is also available for adults riding with children and the chairs can be personalized in a variety of colours.
For many of those coming to the workshop, it is the first time they have had a custom-built mobility aid. They enter the workshop with assistance, but leave under their own steam.
The success of the project is largely due to the determined efforts of Project Director Edouard Norgho. He is a wheelchair user himself and so he fully appreciates the needs of his clients. Ouagadougou has more than two million inhabitants with no public transport systems, so Edouard makes sure that each wheelchair he makes is robust enough to cover long distances every day.
The five wheelchair makers at AMPO are all people with disabilities. Trained on the job, the workshop offers employment to people who often face discrimination on the labour market.
Spreading their expertise beyond the city, staff from the workshop travel further afield to reach up to 1600 people in rural areas. With the support of Rotary Germany the project receives funds and wheelchair parts, helping more and more polio survivors live a mobile life every year.
For the young girl in her new wheelchair, an exciting future awaits. In Burkina Faso more than 70% of children with disabilities have no access to education. Now, able to navigate to school by herself, she can become part of the 30% who do have the opportunity to learn. With the support of Rotary and other partners, AMPO is well on the way to helping more people like her, the target being to provide increased mobility to every polio survivor in Ouagadougou.
To find out more about this project, or provide financial support (US$250 will pay for a wheelchair for a child with disability), please visit sahel.org or contact info@sahel.de.


In Nigeria’s north-eastern Borno state, children displaced by ongoing conflict are being reached with essential immunization and health care services, thanks to a strong network of Volunteer Community Mobilisers established by the polio eradication programme.
Two-year-old Hafsat Khalifa waits patiently in line with her mother, Hadiza. Hadiza is one of many women who’ve brought their young children to receive vital immunization at the local health camp in Maiduguri. Hafsat knows she needs to open her mouth wide when it’s her turn to receive the oral cholera vaccine just like she did when vaccinated with the Oral Polio Vaccine. She displays the confidence of a seasoned pro, although in reality this is the first year she has received any health services, having been born into an area of conflict. Along with these two vaccines, Hafsat will receive other much-needed health care during today’s visit.
Humanitarian crisis
Hafsat is one of many thousands of children affected by the humanitarian crisis in north-eastern Nigeria. The conflict has resulted in a surge in internally displaced persons, with limited access to medical care, leaving millions at risk of life-threatening diseases. Since four cases of wild poliovirus type 1 were detected in Borno in August 2016, an outbreak response for polio has been a top priority. But it has been carried out hand in hand with broader humanitarian efforts to meet the health needs of vulnerable populations.
Benefits beyond polio eradication
UNICEF’s vast network of volunteer community mobilisers have not only played a vital role in ensuring that children like Hafsat receive OPV and other health services every time they are offered, but are leveraging the skill-set they’ve gained from their expanded training to impact child and maternal health far beyond polio.
In addition to receiving the oral cholera vaccine today, Hafsat’s nutrition status will be assessed at the health camp, and children identified as malnourished will be referred for receiving therapeutic food. This important network of polio vaccinators, with years of experience in reaching children with polio vaccines, has made a huge difference in halting the spread of cholera and meningitis outbreaks in Nigeria in 2017. They are also helping create awareness and generate demand for the upcoming campaign against measles.
The reach of this network even extends to protecting children before they are born. Volunteer community mobilisers provide critical antenatal care for pregnant women that can save the lives of mothers and babies alike. And this year, for the first time ever in an emergency humanitarian setting, antimalarial medicines have been delivered on a mass scale alongside the polio vaccine, reaching 1.2 million children in a campaign in August.
For families in Nigeria’s north-east, many who have fled their homes in the face of ongoing violence, this life-line to access essential services is critical to ensuring their children can grow up protected from vaccine-preventable diseases.

The people working to end polio are helping broader humanitarian response efforts in north-eastern Nigeria. With malaria currently claiming more lives than all other diseases put together, a campaign was launched in October to reduce the malaria burden among young children in Borno state by delivering antimalarial medicines. At the same time, community health workers protected children against polio.
“The current campaign marks the first time that antimalarial medicines have been delivered on a mass scale alongside the polio vaccine in an emergency humanitarian setting,” said Dr Pedro Alonso, Director of the Global Malaria Programme, in an interview with WHO on the campaign and the broader humanitarian situation in Borno. “This integrated campaign with WHO’s polio and health emergency teams is an example of unprecedented collaboration to tackle the leading cause of death in a displaced population.”
The humanitarian crisis in north-eastern Nigeria has resulted in a surge in internally displaced persons, with limited access to medical care, leaving millions at risk of life-threatening diseases. In August 2016, four cases of wild poliovirus type 1 were detected in Borno; the outbreak response has been carried out hand in hand with broader humanitarian efforts to meet the health needs of vulnerable populations.
WHO’s well developed network of polio vaccinators, with their years of experience in reaching children with polio vaccines, is making a real difference to the drive against malaria. The polio programme in Nigeria has a vast infrastructure and hundreds of staff on the ground and they are coordinating efforts to make sure that families affected by the crisis have access to other healthcare services.
As a result, the campaigns have reached 1.2 million children with polio vaccines and antimalarial medicines, as shown through a WHO photo story. “I think we will imminently be able to show significant impact,” said Dr Matshidiso Moeti, Regional Director for Africa, reflecting on the encouraging results of the joint campaign.
Read more:
Photo story: Integrated campaign tackles malaria and polio in north-eastern Nigeria

At a meeting of the Group of 7 on 5-6 November 2017 in Milan, Ministers of Health reiterated the importance of sustaining commitment to polio eradication as part of their broader commitment to strengthen health systems. They also recognized… “the importance of continuing our efforts to succeed and keep the world sustainably polio‐free, and, of the opportunity to leverage and transition polio assets and resources that have generated major and broader health benefits, including strengthened health systems.”
At the meeting, entitled “United towards Global Health: common strategies for common challenges”, Ministers discussed key global health challenges guided by the G7 Taormina Leaders’ Communiqué. Their statement on polio was aligned with previous G7 and G20 commitments and with the Sustainable Development Goals.
The attention given to polio eradication by the Ministers forms an integral part of their broader commitment to … “the importance of strengthening health systems through each country’s path towards Universal Health Coverage, leaving no one behind, and of preventing health systems from collapsing during humanitarian and public health emergencies and effectively mitigating health crises”.
Under Japanese and Italian Presidencies in 2016 and 2017, the importance of the global effort to eradicate polio and the opportunity to transition polio-funded assets for Universal Health Coverage and Global Health Security after eradication have been highlighted several times. Such high-level political support for the initiative is critical to maintain the momentum needed for success.
In 2018, Canada, a longstanding GPEI donor, will hold the Presidency of the G7, 16 years after it placed polio eradication on the agenda of the G7 for the first time.
.

Read the original interview here.
For World Polio Day on 24 October, the world celebrated the unsung heroes of the eradication effort. How important have volunteers been in eradicating polio so far?

Volunteers have been and continue to be the backbone of the eradication effort. Local Rotarians are raising critically-needed funds, and members of the community conduct the actual administration of the vaccines on the ground and report cases of paralysis. Without this vast network of volunteers – approximately 20 million strong worldwide – polio cannot be eradicated. They are the true unsung heroes of this effort.
What are the main hurdles to eradicating polio? Are there difficulties getting vaccines to remote communities and areas in conflict?
Those are precisely the main hurdles: reaching children who remain unreached by health systems, because of difficult terrain, conflict, security compromised access, urban sprawl, or large-scale population movements. These are all reasons some children are not vaccinated. The poliovirus is very effective at finding vulnerable children, so we have to be better than the poliovirus at finding that last unvaccinated child. And that is what we are doing with local authorities and partners. Identifying – area by area – the real reasons why children in that area are missed, and then putting in place operational action plans, at the community level, to overcome those reasons. We’re making strong progress: never before has polio been as geographically restricted as it is today. But we are not there yet, and we need to pursue our efforts.
How do you address the challenges of reliable data and identify areas with the lowest immunization coverage?
This is a key issue, particularly at this late stage of the effort, where we really have to focus on reaching the last one or two percent of children who we have so far missed. It is not good enough to achieve 95% coverage nationally, if sub-nationally we are still missing 5%-10% of children somewhere. So we need to be extremely rigorous in the monitoring of our activities, in particular when we assess population immunity levels. We have introduced a number of innovative approaches to address this challenge, such as Lot Quality Assessment sampling, to identify areas which fail to achieve campaign coverage targets; third party monitoring, to get an external view on data quality; and seroprevalence surveys, which show actual immunity levels of children in key areas or high-risk population groups. These tools provide the clearest and most reliable picture of immunity levels.
How can other disease programmes benefit from polio eradication?
Polio eradication has always been about more than polio. Rotary International calls this effort ‘PolioPlus’, with the ‘plus’ standing for more than polio. Polio-funded staff on the ground have been busy helping address other public health emergencies, from the Ebola outbreak in West Africa, the recent drought in the Horn of Africa, to the devastating earthquake in Nepal a few years ago.
Polio-funded staff have also supported Gavi’s immunization efforts, including assisting countries in their implementation of Gavi-funded vaccine and health system strengthening activities. As a concrete example, the proportion of children who have been fully immunized against all vaccine-preventable diseases in some of the most marginalised areas of India increased from less than 20% ten years ago, to more than 80% today.
These broader benefits of the polio eradication effort, however, require that countries and the international

community make sure that the momentum is maintained when polio is eradicated. Indeed, unless this is well planned, the loss of funding coming through the Global Polio Eradication Initiative could negatively impact immunization programmes and other health interventions which have benefited from the large network of staff deployed to eradicate polio. Discussions with partners and countries are underway to map out this process for the post-polio world.
Polio eradication has indeed shown that all children – no matter where they live – can be reached with health interventions. The premise of this programme has been that every child has a right to be protected from lifelong polio paralysis, whether they live in Switzerland, or whether they live in conflict-affected areas of Somalia or areas with limited healthcare infrastructure of Afghanistan. And the lessons and experiences can be – and are being – applied to other disease control programmes.

Harvard University and National Public Radio (NPR) in the United States this month hosted a high-level panel discussion to review how the systematic collection of social data has helped to understand communities and inform and shape strategies to reach every child in the world’s highest-risk polio areas.
The event, titled Eradicating Polio: Reaching the Last Child, featured the Pakistan Prime Minister’s Focal Point for Polio Eradication, Senator Ayesha Raza Farooq, Rotary’s International PolioPlus Committee Chairman Mike McGovern, UNICEF’s polio unit deputy director Jalaa Abdelwahab, and Harvard’s Senior Research Scientist Gillian Steelfisher, in a moderated panel discussion with Jason Beaubien of NPR, which broadcast the forum live.
Since 2013, the Harvard Opinion Research Polling centre has partnered with UNICEF on a collaborative polling effort to support 11 high-quality, strategic knowledge, attitudes and practices (KAPs) polls in seven polio-priority countries, including multiple waves in the remaining polio-endemic countries of Afghanistan, Pakistan and Nigeria.
Hosted in Harvard’s Boston studio before a live university audience, with the video live-streamed on the Harvard Forum website, the Forum speakers described how polling data had underlined the importance of a human-centered approach that placed the frontline worker at the centre of the program, with polling data emphasizing how local, well-trained and motivated frontline workers were the cornerstone for engendering trust in vaccination.
Ms Steelfisher explained that Harvard’s partnership with polio was about generating “data for action – we have to understand the views of the caregivers, what do they think of the vaccine, of the vaccinator. We think this polling puts the ‘public’ in public health.”
Senator Ayesha highlighted Pakistan’s critical innovations of establishing the polio Emergency Operations Centres, the weight given to oversight, monitoring and supervision systems, the need to remain vigilant despite the dramatic reduction to just 5 cases nationwide to date this year, and the importance of strong, evidence-based scientific data to inform the program’s thinking.
“The data informed us to build trust around our vaccinators … to build community ownership. The fact now that polio is considered a locally owned campaign is critical. This last point of eradication is the most difficult to cover and fundamentally it boils down to a question of political will. My Prime Minister has made a commitment to a polio-free world for all future generations and we have no intention of letting them and the rest of the world down.”
Mr Abdelwahab said it was critical to sustain momentum until eradication, not just in the endemic countries but globally. “The ultimate goal is not only eradication but the proof of concept that it is possible to reach every single child. We need to sustain the appetite of communities all the way to certification (of a polio-free world) via the human-centred approach and community-based vaccination.”
To watch The Forum, go to: https://theforum.sph.harvard.edu/events/eradicating-polio/

It’s a clear, summer day in Safdarabad, in the Punjabi province of Pakistan, and Mr. Patras Maseeh Bhatti and his colleagues have just arrived at “work” for the day. Surrounded by brick buildings instead of the inside of laboratory, they might look out of place in their attire. Dressed from head to toe in bio-hazard lab coats, long black rubber boots, and thick industrial gloves and armed with a bucket, their mission is to collect enough sewage from the selected sample site to be transferred in a separate container to the laboratory in Islamabad. Once there, the sample will be tested for poliovirus.
This sampling is part of a system of disease surveillance, which underpins the entire global effort to eradicate poliovirus. Without surveillance, it would be impossible to pinpoint where and how wild poliovirus is still circulating, or to verify when the virus has been extinguished from the wild.
Across the Eastern Mediterranean Region, disease detectives like Mr. Bhatti are becoming more and more important in the fight to end polio. In addition to surveillance for Acute Flaccid Paralysis (AFP), which involves the detection and reporting of children with rapid-onset ‘floppy’ limbs, environmental surveillance involves testing sewage or other environmental samples for the presence of poliovirus.
“This is the only mechanism where you will be able to detect viruses that are circulating with the absence of paralytic polio cases,” Dr Humayun Asghar of WHO’s Regional Polio Programme explains. “As we get closer to eradicating polio even with very high [vaccination] coverage in the population, the virus can still circulate undetected in under-immunized children.”
The growing network of disease detectives
Although AFP surveillance remains the gold standard for surveillance for polio, only one in approximately 200 cases of polio actually show symptoms of paralysis. The World Health Organization has been working closely with a number of countries within the Eastern Mediterranean Region to expand environmental surveillance networks and build capacity in field and lab staff. In endemic areas, environmental surveillance is providing critical supplemental information and data, enabling epidemiologists to tailor the eradication strategies even further. In other parts of the Region, it is proving a critical additional tool to mitigate the risks of a potential virus importation, particularly given the challenges that some countries face, including large-scale population movements, inaccessibility or insecurity.
“In these situations, any additional tools to supplement our AFP surveillance are critically valuable,” he says, “and we need a robust system in place for countries to be able to manage this network.”
In countries like Pakistan and Afghanistan, Dr Asghar says rapid and extensive population movement is the biggest risk for the virus spreading. “The virus moves with the people, so we cannot be sure that the virus is staying where we detect the cases. Here, environmental surveillance has proven extremely valuable because in the absence of many paralytic cases, we continue to detect wild poliovirus in the environment which tells us a lot about how and where the virus might be continuing to hide.”
The detection of poliovirus in countries not recording paralytic cases is also very useful, Dr Humayun says. During the polio outbreak in the Middle East in 2013-2014 this helped to inform partners carrying out the multi-country regional response where to further concentrate efforts in order to close the outbreak and ensure it did not spread further.
In both Pakistan and Afghanistan, environmental surveillance has been one of the key strategies for narrowing in on where the virus continues to circulate, and the lessons learned through the establishment of environmental surveillance in these countries is informing the expansion across the region.
In Lebanon and Jordan, where environmental sampling has been established in 2017, staff have been trained to collect samples from specified collection sites and to ensure the samples reach the laboratory in Amman in the right condition for processing.
Efforts to build on existing health infrastructure and disease surveillance systems in Iran, Sudan, Somalia, Syria and Iraq are underway, with plans for the expansion of environmental surveillance systems and lab networks in 2017.
Leaving a lasting legacy for health systems
Since the Global Polio Eradication Initiative (GPEI) began in 1988, the programme has mobilized and trained millions of community health workers and volunteers for surveillance. A standardized, real-time global surveillance and response network exists and is being put to full use.
Dr Humayun says that this investment in people and infrastructure is not only of benefit during the last mile of polio eradication, but will be a lasting legacy that the polio programme will leave behind for health systems of countries across the region.
“Polio surveillance methods, techniques, facilities and knowledge are our biggest assets, but they have applications beyond our programme. So, these laboratories can be of great value then to countries who need to develop their capacity in other diseases of public health importance,” he says.
Learn more about disease surveillance
A force of determined women already involved in the fight against polio has been assembled to lead work to curb the spread of a cholera outbreak in northeast Nigeria. Displaced by conflict and themselves living in camps around the crisis region, these women are moving from tent to tent to help families understand the risks they face during the rainy season, and how to get help if they fall ill.
Volunteer community mobilisers are often the only way community members know how to keep their families healthy in the face of extreme hardship.
These dedicated volunteers provide their neighbours with this vital service while facing their own hardships brought on by displacement.

“Are you watching me?” “Yes, ma’am.”
“Are you seeing me?” “Yes ma’am.”
Along two rows of benches under the awning of the Chikun Primary Health Centre in northern Nigeria’s Kaduna State, about 50 young mothers sit still, their babies swaying on their laps. All eyes are fixed on Lidia, the assured polio social mobilizer who is not delivering polio vaccine, but showing the women how to correctly breastfeed.
Lidia is a grandmother, a one-time community midwife now employed with Nigeria’s polio eradication programme as a UNICEF-supported Volunteer Community Mobilizer (VCM). During the monthly polio vaccination campaigns, she goes house to house with the vaccination team, opening doors through her trusted relationship with the mothers, tackling refusals where they occur and tracking any children missed in the campaigns through her field book containing the names and ages of all children in her area. But it is between campaigns where Lidia’s full worth is realized.
Trust
Helen Jatau, a supervisor in this Local Government Area, supervises 50 VCMs and five first-level supervisors. She is convinced the health care polio frontline workers provide between campaigns provides benefits beyond the surface value – it establishes trust. “When we bring different things to the mothers, it helps the community live better and even accept us more, because we are giving more than just polio vaccines.”
Between polio vaccination campaigns, mobilizers like Lidia track pregnant women and ensure the mothers undertake four Ante-Natal Care visits, including immunization against tetanus. They advise mothers-to-be to give birth at the government health facility, provide them with the first dose of oral polio vaccine, facilitate birth registration and connect them to the routine immunization system. In houses and at monthly community meetings, the mobilizers also provide information on exclusive breastfeeding, hand washing, the benefits of Insecticide Treated Bed Nets, Routine Immunization and the polio vaccination campaign.
Ante-Natal Care
VCM Charity Ogwuche stands before the mothers at the health centre and peels over the pages of a colourful flip book. “Breastmilk builds the soldiers inside your child,” she shouts. “It will save you money. You don’t need to find food for your child to eat. You don’t need to find water: 80% of breastmilk is water. It will protect your child.”
Adiza, a young mother holding her first child, Musa, carries a routine immunization card including messaging on breast feeding and birth registration. “Aminatu talked to me about antenatal care. She asked me to get the tetanus shot, and today she has brought me here to receive routine immunization for my baby. I am really grateful. If she wasn’t here I wouldn’t be here. I wouldn’t know about it. She is the only one who tells me about this.”
Charity is proud of her work. “The women are so familiar with me, it makes me happy. They call me Aunty. I provide most of the health information for them. Really there is no other in our community. They are very young mothers and they need me.”
Birth registration

Every Tuesday is birth registration day. Once, hardly a soul turned up to register their newborns, but today, a long line of VCMs are standing clutching handfuls of registration forms, waiting to register the newborns within their catchment area.
Aminatu Zubairu, wrapped in the trademark blue hijab of the VCM, explains how all social mobilizers must come from their own community, and how that familiarity breeds the trust that has enabled her to register hundreds of children in her area. “I go to their houses and ask if they had the birth registration. If they say no I take all the information. Now I will register them and get the certificate of birth and carry it to their house to give back to them. In a month I can do 50 of these. This year there are plenty of newborns.”
Danboyi Juma, the district’s Birth Registration Officer, believes birth registrations have increased by 95% since VCMs assumed responsibility for the service. “They are helping us so much because they go house to house,” he says. “They have increased the number of birth registrations in this area by so much – oh, that’s sure.”
Routine Immunization

Despite stifling heat, on this Tuesday, there are more than 50 mothers and several fathers sitting on benches, waiting for their turn to have their babies vaccinated. More than 80% of them carry the cardboard cards given to them by VCMs to remind them their baby is scheduled for routine immunization.
Jamila, a young mother wrapped in a white shawl around her orange head-dress, is bringing her six-month-old baby Arjera to be vaccinated for the first time. Her VCM, Rashida Murtala, badgered her for months before Jamila finally accepted.
“Oh, she refused and refused,” Rashida says. “She’s fed up with me visiting. I went to see her today and finally she followed me. I’m happy to see her here.”
Jamila smiles. “She has been disturbing me every day that I have to take this child to the health centre. I know she’s right, so today I followed her.”
Priscilla Francis, the Routine Immunization provider who vaccinates young Arjera, believes VCMs are key to strong vaccination coverage in Chikun district. “There is much improvement in attendance since the VCMs started. They are well trained. They do a good job of informing mothers to come. If we lost them we would lose our clients – no doubt. When they come we tell them to come back, but no one else is going to their house to bring them.”
Hassana Ibrahim, a Volunteer Ward Supervisor, knows her mobilizers are important. “I have 10 VCMs, five in this ward. Non-compliance used to be a big problem but not now. Now with the routine immunization, the community sees they are providing a package of health care and now people comply with the polio vaccination.”
Naming ceremonies

Following the routine immunization session, the VCMs fan out to attend the naming ceremonies of newborns in their catchment area. Naming ceremonies provide an important opportunity to vaccinate lots of children, as family gathers around to celebrate. On average, they attend 10 naming ceremonies a month. Today we visit Naima, the young mother of a 7-day-old boy, who as per tradition has just been named Jibrin by his grandfather. Naima is surrounded by her sisters, family and village friends, who cook and eat with them, and their 68 children under five. Within minutes, the VCM has walked among them all, vaccinating them as they sit waiting with their mouths open to the sky like little birds.
Naima is happy to see her trusted VCM, and encourages her to vaccinate the children. “I know her well,” she says. “She taught me to go for ante-natal care, to deliver at the hospital and to go for immunization. She is the only health care worker who comes. We are from the same community. She is my friend.”