Eradicating polio is a particularly unforgiving task. While the virus remains anywhere in the world, it has the potential to spread around the globe to any vulnerable child or community. As the Global Polio Eradication Initiative (GPEI) zeros in on polio, it becomes more important than ever that every last virus is found and rapidly stopped in its tracks. In this photo series, Dr Ousmane Diop describes how environmental surveillance is one of the innovations being used to find every last strain of poliovirus in every last corner of the globe.
Traditionally, the polio programme uses acute flaccid paralysis (AFP) surveillance for rapidly detecting where polio is present. This process involves using a wide network of health workers, teachers, traditional healers and families to find and report children who have symptoms that could be polio: floppy, rapid-onset paralysis with no obvious cause. Stool samples of people with these symptoms are tested in laboratories to see whether they are the result of the poliovirus, and in the case of a positive result, an outbreak response is launched or efforts strengthened in the area where the case was found. In order to ensure polio surveillance is sensitive enough, endemic countries are required to find and report at least two cases of AFP per 100,000 people aged under 15 years of age. This is the number of AFP cases that you would expect to find in a given population, regardless of whether polio is circulating or not. In this way, if poliovirus is present and causing the cases of paralysis, it will be rapidly detected and can be addressed.
Why environmental suAFP surveillance brought us a great distance towards eradication. But approximately only one in two hundred people infected with poliovirus show symptoms; in most cases, there is no visible sign that the virus is present. This means that at any one time, the virus could be silently beginning to circulate amongst children, without being picked up by AFP surveillance. Poliovirus is spread through faeces, and once an individual is infected they can shed it for several weeks. Environmental surveillance therefore gives us an important tool to gather information about where the virus is, even when no case of paralysis gives it away. Testing sewage generated by populations where polio is likely to be present provides a method of looking for the virus in many thousands of individuals at once, rather than one at a time.rveillance?
Countries are chosen for environmental surveillance based on multiple factors. Areas with poor AFP surveillance rates, that are particularly prone to poliovirus circulation, or where the virus comes back again and again are particularly good candidates. Even in low-risk areas, environmental surveillance can act as an early warning system to check for wild polio or even to see whether the weakened virus in the oral polio vaccine is changing into vaccine-derived polioviruses.
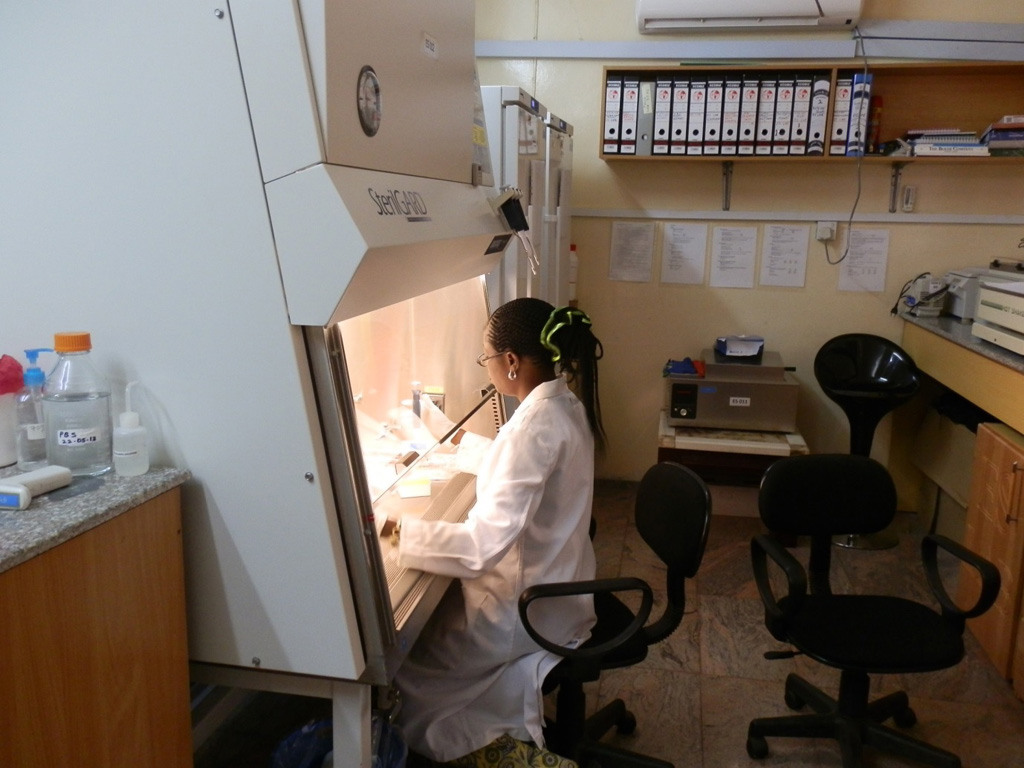
Following a decision in support of environmental surveillance, it often takes at least 3-4 months to build the required laboratory capacity. Staff must be trained and the relevant security measures put in place to ensure there is no release of bio-hazardous materials.
Once the laboratory infrastructure is in place, on-site training is carried out to equip the field and laboratory workers with the information they need to carry out environmental poliovirus surveillance. Experts like Ousmane take the technicians to the field to show them best practices for choosing sample sites and how to collect samples.
In poor resource settings, there is no structured wastewater network. From individual houses, wastewater runs into channels where the sewage of whole communities gathers. The best sampling sites are from places like this, where sewage samples may represent tens to hundreds of thousands of people.
Open drains are the usual places to gather samples. Surveillance officers visit sites in the early morning, when there is a higher flow of sewage. In warm climates, starting early in the day ensures that hot weather will not damage the virus before it can be tested.
In order to collect environmental samples, safety gear including water-proof gloves, appropriate boots and face masks must be worn. The sample is dispensed into a sealable container, which is carefully wrapped up in even more layers of protective materials to keep the potential virus contained. When the surveillance officers remove their gloves, they have to be make sure that the outside does not come into contact with the skin, and that they carefully wash their hands afterwards.
Once samples are collected, they are immediately labelled, refrigerated and transported to the laboratory using a reverse cold chain, due to the importance of ensuring the virus does not denature in the heat. Samples are inspected within 48 hours of collection. As a first step, the samples are then concentrated down and purified.
Following concentration, the specimen (which may or may not be positive for poliovirus) is introduced to some cells which are susceptible to poliovirus. The cells are left for a few days. If the specimen does contain poliovirus, a structural change in the host cells can be seen when viewed under a microscope.
In the event of polio being detected in the environment through this process, the information is used to plan vaccination campaigns, so that children are protected before anyone can be paralysed. Environmental surveillance will continue to be important for many years into the future. After eradication, environmental surveillance will be used to check no virus is released from laboratories or research facilities that could cause an outbreak. Environmental surveillance is made possible, under WHO coordination, by the generous funding of Canada, the Korea Foundation for International Healthcare, the US Centres for Disease Control, the Bill and Melinda Gates Foundation, Rotary International, Switzerland and the UK’s Department for International Development. It is becoming increasingly important as we zero in on the final cases of poliovirus, making sure that one day soon, no child will ever be paralysed from poliovirus again.